The low blood oxygen levels of obstructive sleep apnea (OSA) cause widespread changes in gene activity throughout the day, according to a new study published in PLOS Biology. The finding may lead to tools for earlier diagnosis and tracking of the disorder.
The activity of many genes varies naturally throughout the day, partially in response to activity of circadian clock genes, whose regular oscillations drive circadian variation in up to half the genome. Gene activity also varies in response to external factors, including decreases in oxygen levels, which causes production of “hypoxia-inducible factors,” which influence activity of many genes, including clock genes.
To better understand how OSA may affect gene activity throughout the day, the authors exposed mice to intermittent hypoxic conditions and examined whole-genome transcription in six tissues—lung, liver, kidney, muscle, heart, and cerebellum—throughout the day. The authors then evaluated variation in the circadian timing of gene expression in these same tissues.
The largest changes were found in lung, where intermittent hypoxia affected transcription of almost 16% of all genes, most of which were upregulated. Just under 5% of genes were affected in heart, liver, and cerebellum. The subset of genes that normally exhibit circadian rhythmicity were even more strongly affected by intermittent hypoxia, with significant changes seen in 74% of such genes in the lung and 66.9% of such genes in the heart.
Among the genes affected in each tissue were known clock genes, an effect that likely contributed to the large changes in circadian activity of other genes seen in these tissues.
“Our findings provide novel insight into the pathophysiological mechanisms that could be associated with end-organ damage in patients with chronic exposure to intermittent hypoxia,” says study author David Smith, MD, PhD, of Cincinnati Children’s Hospital Medical Center, in a release, “and may be useful to identify targets for future mechanistic studies evaluating diagnostic or therapeutic approaches.” These, for instance, could be through a blood test tracking one of the dysregulated gene products to detect early OSA.
Study author Bala S. C. Koritala, PhD, Cincinnati Children’s Hospital Medical Center, adds in a release, “Our study using an animal model of obstructive sleep apnea unveils time- and tissue-specific variations of the whole genome transcriptome and associated hallmark pathways. These unique findings uncover early biological changes linked to this disorder, occurring across multiple organ systems.”
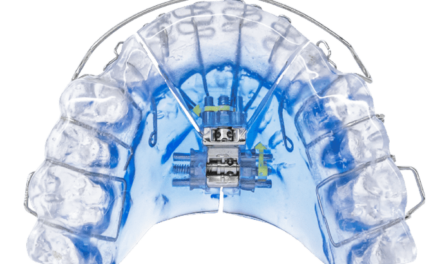
Photo caption: Obstructive sleep apnea disrupts gene activity throughout the day in mice.
Photo credit: Bala S. C. Koritala