Patients’ last days of COPD can be characterized by depression, anxiety, pain, and dyspnea. Clinicians must be alert to patient discomfort and offer appropriate palliative care and reassurance.
By Tim Nuccio and Paul Nuccio, RRT, FAARC
Editor’s Note: Written by RRTs Paul Nuccio and Tim Nuccio, 2009’s “Give Them Comfort: Controlling COPD Symptoms at the End of Life” has consistently been one of RT magazine’s most popular articles, ranking in the top two in online views every month. Eight years later, the Nuccios have written a follow-up article that offers new recommendations for palliative care and reflects on the progress in end-of-life care for patients with COPD, a disease that is now the #3 cause of death in the United States. Part II is available here.
Considered as a long course of chronic disease that is characterized by repeated exacerbations and remissions, chronic obstructive pulmonary disease (COPD) indisputably leads to a clear and steady decline.1 For the purposes of this paper, focus will be given to the two diseases that are considered to be the hallmark of COPD: chronic bronchitis and emphysema. More specifically, this article will explore various methods for controlling the sometimes devastating symptoms associated with COPD toward the end of life.
When the patient gets to these “last days,” careful attention to symptom control can prevent, minimize, or eliminate distress, thus improving the quality of life until the time of death. In addition to exploring methods of reducing the suffering that is experienced by the patient, attention will also be directed at the importance of considering family members and loved ones during this difficult stage of the deadly disease. Since COPD is a progressive disease as opposed to a curable one, focusing our energies and resources on symptom control is the best way that we as health care providers can serve these patients.
Rising Mortality Rate
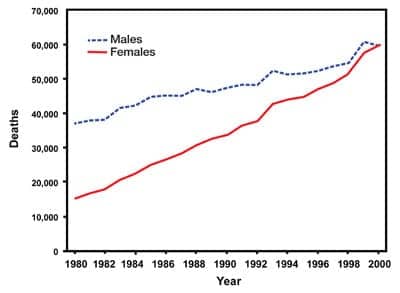
According to the Chronic Obstructive Pulmonary Disease Surveillance Report,2 published in the Morbidity and Mortality Weekly Report in 2002, that looked at the mortality rate from the years 1971 through 2000, COPD deaths rose steadily each year. Particularly interesting in this report were the differences in death rates between men and women. Although both males and females have shown increases in their death rates each year, female deaths have increased at a more dramatic rate, and by the year 2000 had nearly surpassed the death rate of males (Figure 1).2
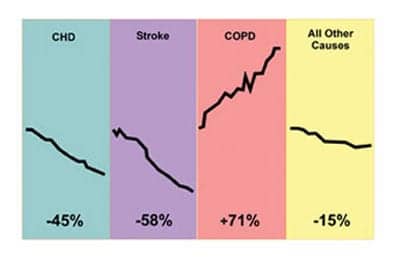
The costs associated with COPD are staggering, with in excess of $30 billion spent annually. The average Medicare expenses for patients with the disease are 2.5 times greater than for those without the disease. COPD is currently the fourth leading cause of death in the United States and is expected to move to the number-three position by the year 2020. Approximately 112,000 people died of COPD in 1998 alone, and the mortality rate of COPD continues to rise each year (Figure 2).3
Within the final year of life, COPD patients will typically have an FEV1 of less than 30% of predicted, a declining performance in their activities of daily living, and an uninterrupted-walk distance of only a few steps. The patient usually will have at least one urgent hospitalization within the previous year, have left-heart and/or other comorbid diseases, and show signs of depression. These patients are generally elderly, and many are unmarried. The divorce rate among those patients with COPD has been shown to be increased compared to those without the disease.1,4
Assessing the Symptoms
In the final days or hours of patients with COPD, symptoms such as hypersomnolence, disorientation, irregular breathing patterns, mottled skin, cool extremities, reduced production of urine, and generally altered vital signs are all observed. Retained secretions in the upper airway are also quite common, as is a reduced interest in food and/or water.
Strong patient assessment skills are of vital importance when caring for the COPD patient. Failure to recognize symptoms, and thus not providing relief for such symptoms, does a significant disservice to these patients during their final days. Patients in this condition have difficulty accurately describing their symptoms, and the subjective nature of self-reported symptoms often makes them difficult to decipher. Clinician accuracy when reporting a patient’s symptoms has also been found to be poor. Utilization of a symptom measurement tool must be considered when caring for these patients.
A variety of symptom-measurement instruments have been developed and are now used to assess the COPD patient. Three of the more common tools are the Memorial Symptom Assessment Scale (MSAS),5 the Rotterdam Symptom Checklist (RSC),6 and the Visual Analog Scale (VAS).7 Formal dyspnea assessment tools are also used.
There are barriers to the assessment of symptoms, because patients with advanced disease typically suffer with fatigue, depression, and delirium. Many, if not most, of these patients experience more than one symptom, making assessment difficult. Other barriers include the fact that caregivers are frequently not willing to take the time necessary to gain a thorough understanding of the patient’s symptoms, and the disease itself and its progression are often difficult to discuss for both patients and caregivers.
In a study that evaluated the perceptions of family members regarding the most severe symptoms that their loved one had experienced during their final 3 days prior to death, dyspnea, cough, pain, and confusion, in that order, were rated as being the most significant, with more than 90% of them rating dyspnea as the most severe.8
Other common distressing symptoms associated with COPD are anxiety, depression, and anorexia/cachexia. When contemplating the management of these symptoms, we should consider general principles of palliation and determine and treat the underlying cause of the symptoms whenever possible. When attempting to relieve symptoms, clinicians need to pay careful attention to avoid the addition of any new problems. We need to give careful consideration as to whether our treatment is worthwhile for the patient as well as their family, and it is important to discuss all reasonable treatment options with both the patient and family.
Breathless
According to the National Lung Health Education Program (NLHEP),9 “dyspnea, the sensation of breathlessness or inadequate breathing, is the most common complaint of patients with cardiopulmonary diseases.” Dyspnea occurs when an imbalance exists between the perceived need to breathe and the perceived ability to breathe. It is the “experience” of shortness of breath, and it may or may not be associated with suffering. Dyspnea is often associated with panic and anxiety. The panic may present as dyspnea, while dyspnea may induce panic.
When trying to identify dyspnea, oxygen saturation is not a reliable indicator, and a patient’s own report or signs of agitation or anxiety are considered the best means of identifying dyspnea. The patient who is dying of COPD or lung cancer will typically experience a worsening in their dyspnea level as their disease progresses. In addition to the previously discussed panic, fear, and anxiety, patients may also become depressed and angry.
Causes of dyspnea in the COPD patient include such things as airway obstruction or restriction, hypoxemia, and deconditioning of the respiratory muscles. Cardiovascular issues such as congestive heart failure or cor pulmonale can also result in dyspnea. Anxiety, fear, anemia, and fluid overload may equally contribute to the symptom. The ability to control dyspnea in end of life COPD patients is of tremendous importance for these patients and their families.
Easing the Symptoms
Pharmacotherapy options for controlling dyspnea vary, depending on the specific cause for the discomfort. Bronchodilators are frequently given to the COPD patient to relieve bronchospasm. For the patient who develops CHF, diuretics can be helpful in reducing excess fluid. Opioids have shown some benefit in reducing dyspnea, with oral administration being the preferred route. Oxygen therapy is used when indicated and tolerated. For the patient who experiences anxiety, benzodiazepines are often used. Phenothiazine, an antipsychotic drug, may be used in cases of severe agitation. Anti-inflammatory side effects are not usually an issue during end of life care, therefore the use of corticosteroids is not generally indicated.
Much attention has been given to the use of inhaled/nebulized opioids, with most positive outcomes being based on anecdotal experiences. It is thought by some that inhaled opioids may act directly on lung afferent nerves, thus altering the perception of breathlessness. It is believed that they may diminish the response to hypoxia and hypercapnia at the chemoreceptor level or may exert a peripheral effect on opioid receptors in the lung. It is important to note that nebulized morphine may cause histamine-mediated bronchospasm during the first nebulization, so caution should be taken to ensure that treatment for bronchospasm is readily available.
Of 30 studies that were found in a PubMed review, only two prospective, randomized, double-blinded, placebo-controlled trials have examined the efficacy of aerosolized opioids on dyspnea in patients with advanced disease. Noseda et al10 found no benefit from 10 mg or 20 mg of aerosolized morphine citrate in treating dyspnea in 17 patients with severe chronic lung disease or metastatic cancer. Bruera et al11 found that aerosolized morphine sulfate given to patients with metastatic cancer was as effective as that given subcutaneously. Why the large discrepancy in the two studies? A possible explanation may be that in the Noseda study, 12 out of the 17 patients had COPD and only three had metastatic cancer. Two of the three with cancer died, and their data was not included. The Noseda investigators assessed dyspnea 10 minutes after completion of nebulization, which may have been an insufficient amount of time.
According to a paper by Kallet,12 higher-level clinical evidence consistently shows that aerosolized opioids are not effective in improving dyspnea or exercise tolerance in patients with chronic cardiopulmonary diseases, including COPD and idiopathic pulmonary fibrosis. Low level clinical evidence supports use of aerosolized opioids for palliation of dyspnea in patients with advanced cancer and cystic fibrosis. Low level clinical evidence also suggests that aerosolized furosemide may reduce dyspnea in both groups of patients.
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD),13 oral and parenteral opioids are effective for treating dyspnea in COPD patients with advanced disease. There is insufficient data to conclude whether nebulized opioids are effective. However, some clinical studies suggest that morphine used to control dyspnea may have serious adverse effects and its benefits may be limited to a few sensitive subjects.
In terms of dyspnea treatment principles, opioids and benzodiazepines are considered by some to be the mainstays of palliative therapy for dyspnea. Which one is more effective? A patient who complains of difficulty breathing but who lacks associated anxiety is more likely to benefit from an opioid. A patient who complains of anxiety associated with breathing might be better treated with a benzodiazepine, at least initially. Many patients will require both types of medications.
In addition to pharmacological treatment of the symptoms of dyspnea, there are also nonpharmacological methods that have been shown to benefit some patients. These include such things as elevating the head of the bed, massage therapy, relaxation therapy, and pursed-lip breathing. Many end of life COPD patients find that using a fan provides them with a certain level of relief. According to a study at Johns Hopkins, fans improve dyspnea by stimulating receptors in the trigeminal nerve located in the cheek and nasopharynx, altering the perception of breathlessness.14
Easing the Pain
Pain control can be an issue for these patients, although most pain can be alleviated with medication use. It is best to administer pain medications on a regular basis, as opposed to allowing them to wear off. Waiting until the patients request the medications could result in a delay in their administration and an exacerbation of the pain. This may lead to increased anxiety for both the patients and their families.
Another issue that must be addressed when caring for these patients is that of cough control. Although cough is a normal protective mechanism, it may also be induced by such things as infection, reflux, aspiration, and airway disease. Cough may also be drug-induced. Expectorants and mucolytics have been found to be ineffective, while oral narcotics, such as morphine and codeine, have been shown to provide some relief. Nebulized lidocaine has been used in cases of severe cough, although this may increase the patient’s risk of aspiration.
During the final 24 to 48 hours of life, patients may demonstrate what is commonly known as “death rattle.”15 This is a sound that is caused by airflow passing through secretions that accumulate in the back of the throat. Although at this point the patient is usually unaware that this is occurring, family members as well as staff may find this to be distressing. Education of family members is important, and repositioning the patient may be helpful. Oropharyngeal suctioning, although it may be helpful, should be avoided if it causes the patient to gag or cough. The use of anticholinergic drugs may be helpful if used prior to the buildup of secretions.
Of the utmost importance for these patients is that they are made as comfortable as possible. All patients with a terminal condition, such as end of life COPD, should be provided access to palliative care services. The National Consensus Project for Quality Palliative Care16 states: “Palliative care is both a philosophy of care and an organized, highly structured system for delivering care. The goal of palliative care is to prevent and relieve suffering and to support the best possible quality of life for patients and their families, regardless of the stage of the disease or the need for other therapies.” This specialized care is delivered by an interdisciplinary care team that includes such professionals as physicians, nurses, respiratory therapists, physical therapists, nutritionists, pharmacists, chaplaincy representatives, and other health professionals.
The previously mentioned consensus guidelines further state: “Palliative care affirms life by supporting the patient and family’s goals for the future, including their hopes for cure or life-prolongation, as well as their hopes for peace and dignity throughout the course of illness, the dying process and death. Palliative care aims to guide and assist the patient and family in making decisions that enable them to work toward their goals in the course of one’s illness, condition or injury.”11
Role of Respiratory Therapists
As part of the palliative care process, respiratory therapists may recommend providing, or be requested to provide, oxygen therapy, bronchodilators, secretion clearance techniques, noninvasive ventilation, pulse oximetry and capnography monitoring, as well as communication with the patient and family members. The respiratory therapist is also in a position to provide support and reassuring words, and perhaps even hand-holding, during the final days and hours of the patient’s life. We may be unable to cure these patients of their devastating disease, but we can all play a significant role in the relief of symptoms, and in providing our patients with the respect, care, support, and comfort that they deserve.
RT
Tim Nuccio is an RT student at North Shore Community College in Danvers, Mass. Paul Nuccio, RRT, FAARC, is director of pulmonary services at Brigham and Women’s Hospital in Boston. For further information, contact [email protected].
References
- Sorenson HM. 2005. Controlling COPD Symptoms at the End of Life. Available at: www.aarc.org/education/webcast/archives/end_of_life/04.19.05. Accessed January 19, 2009.
- Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic Obstructive Pulmonary Disease Surveillance—United States, 1971-2000. Morbidity and Mortality Surveillance Summary. August 2, 2002. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/ss5106a1.htm. Accessed January 12, 2009.
- Higgins MW, Thom T. Incidence, prevalence, and mortality: intra- and intercountry differences. In: Hensley MJ, Suanders NA, eds. Clinical Epidemiology of Chronic Obstructive Pulmonary Disease. New York: M Dekker; 1989:23-43.
- Hansen-Flaschen J. Chronic obstructive pulmonary disease: the last year of life. Respir Care. 2004;491:90-8.
- Portenoy RK, Thealer HT, Kornbilth AB, et al. The Memorial Symptoms Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and desires. Eur J Cancer. 1994;30A:1326-36.
- deHaes JCJM, Olschewski M, Fayers P, et al. The Robberdam Symptom Scale. Available at: www.rug.nl/gradschoolshare/research_tools/assessment_tools/rscl_handleiding.pdf. Accessed January 19, 2009.
- National Cancer Institute. Dictionary of Cancer Terms. Visual analog scale. Available at: www.cancer.govb/templates/db_alpha.aspx?CdrD=46784. Accessed January 19, 2009.
- Lynn J, Teno, JM, Phillips RS, et al. Perceptions by family members of the dying experience of older and seriously ill patients. Ann Intern Med. 1997;126:97-106.
- Frontline assessment of common pulmonary presentations. National Lung Health Education Program (NLHEP). Available at: www.nlhep.org/books/pul_Pre/dyspnea.html Accessed January 12, 2009.
- Noseda A, Carpiaux JP, Markstein C, Mayvaert A, de Maertelaer V. Disabling dyspnea in patients with advanced disease: lack of effect of nebulized morphine. Eur Respir J. 1997;105:1079-83.
- Bruera E, Sala R, Spruyt O, Palmer JL, Zhang T, Willey J. Nebulized versus subcutaneous morphine for patients with cancer dyspnea: a preliminary study. J Pain Symptom Manage. 2005;29:613-8.
- Kallet RH. The role of inhaled opioids and furosemide for the treatment of dyspnea. Respir Care. 2007;52:900-10.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD), 2006. Available at: www.goldcopd.com. Accessed January 12, 2009.
- Enck RE. The Medical Care of Terminally Ill Patients. Baltimore: Johns Hopkins University Press, 1994.
- Dean MM. End-of-life care for COPD patients. Prim Care Respir J. 2008;17:46-50.
- National Consensus Project for Quality Palliative Care, 2009. Available at: www.nationalconsensusproject.org/WhatIsPC.asp. Accessed January 12, 2009.









My 73 year old father has copd hes been in intensive care twice in last month and on ventilator twice in that time he’s so frightened looking it’s heartbreaking to see him like this ,do you think he is in final stage of copd ?
It might be the third of last. Im so sorry. I’m going through the same thing with my nana.
I’m so sorry for both of you. I hope both your parents are still alive. My dad is in icu today. Not sure how the outcome will be. X
My grandfather suffered from copd, notably the last 8 months of his life. He was in and out of the hospital at least 4 times before he passed on Father’s Day this year. The depression was very evident as he was a very active man his entire life leading up to his death. He was scared up until his final days of death. I was fortunate enough to see him the day before he passed where he looked ok but was talking about wanting to die and he was just sad living a life that had him hooked to an oxygen tank and a nebulizer. I miss him everyday and love him very much. I’m at peace his suffering is over as this disease destroyed his quality of life.
Very sorry for your loss, Joe.
Hello my name is Mike I have been diagnosed with chronic lung desease stage 2 from being rushed to hospital with lack of breath since admitted all tests taken and showing that lung are falling at speed to quickly I was given all new medication forstair maxinhalors to try to slow process but hospital tells me that time scale I will live will be within 4months to max 10months I was only diagnosed with this illness on 27th October 2020 and I’m only aged 44 with this chonic lung desease it’s now increase in stage due to lung showing failing from date 27th October when diagnosed to January 1th 2021 by 40 ‘/’ failing lungs given my illness they shows I will nlow have full chonic lung failure and I will go into cardiac arrest and no response within 10 months from the date pronoced effect to my self I thought I would share this information do everyone will get more aware that COPD disease has not cure in mefication only medication will slow process of it’s damage to lungs BUT not cure all People shown having COPD will know same outcome to there lifel in last stage , thankyou for reading this message
So sorry 4 ur loss. Its a hard road for both patient n familys. watching them suffer. Ur Dad must of been great Dad too pass on Fathers Day. U will never forget him . R.I.P. Dad.
I am suffering this horrible disease and am so tired of the pain. I finally got healthcare in a program here in Topeka KS called PACE. it is wonderful and the doctors do not adhere to the same rules as those Doctors in Society who fight us with chronic pain and relief issues basically calling us drug seekers and such things like that. I have wasted all the good years that I had left before ending up a lump on my couch overweight and alone. Shame on them after reading this I feel so informed and now ready to confront my end of life issues. I am so grateful for this new program I am in. they are great and do not make us feel as if we are begging or if we are a bother. I got PTSD from going to doctors as they lied to me about my condition and now it is too late I am so angry at them but thanks to my new doctor, also Meals on Wheels along with medication and Oxygen with all my needs met without the hostility that was offered to me as a disguised healthcare. After reading this I am enlightened and feel that my last days will be with EYES WIDE OPEN and no more of this hiding the truth or passing the buck for my diagnosis. This is all I ever wanted was a diagnosis and a plan to get the most out of life while I was able to enjoy it. I see me in so much of the actions that they describe about our condition in the last months and days of our existence as a fellow human being on planet Earth.
I am finally as pain free as I can be and I am not having to beg for my medications .. the meds are called medications and not DRUGS what a deal. If you are in pain like me the pills go to the pain not the brain.
I could do a documentary on my end of life issues and how I was treated by doctors and therapists Nurses and hospitals. I hope that if someone who suffers like me and finds this site that my story will help you seek a program for those folks 55 and older albit to emotionally disturbed or mentally disabled or just plain old tired of being in pain and living with it. I was shocked at the ease of me getting rid of my pain What a glorious end of my road to the end of my life issues I am not sure where I stand but I am having DYSPNEA at this time I just got back on my pain medications only at 15 mg Morphine tab long lasting and break thru 15 mgs quick action Morphine 3 a day and 4 for the long lasting. I use oxygen and watch my breathing. I do not suffer lots of other medical condition and trust me when I tell you that I got his lung damage from a chemical spill when I was 30 yrs old working in Tucson AZ. for 3.10 per hr job in which I wasn’t hired full time and after the spill the owner let me go well I got 25% lung damage right off the bat. eventually another 25% then developed a progressive wasting away of my lung tissue. All for 3.10 an hour. I am 65 now and was in great shape last May until the doctor I had did not feel comfortable giving me my pain medications and she cut me off and after 10 years with a relative low dose of 2 60 mg Morphine long last and 15 MG breakthru Morphine along with Diazepam at 10MGs at 4 times per day .. this is low for my condition .. as a result I became inactive a lump on my couch as my house fell apart around me . I did not get bathed properly nor did I clean house and as I told my doctor Last May I was mowing my own lawn. I feel that due to this neglect I have damaged myself to the point of where I am at now.
I can only hope that my health recovers but if this is it…the end I would love to know. if not and I do have more time so be it and I will do my best to make sure I am not around second hand smoke or any irritants that cause me to be more sick
thank you for this site and the knowledge that I have learned as well to allow me to talk better to my new doctor who I might add is wonderful and caring and doesn’t mind that I am smart and tuned in to my own health issues .. she told me Doctors either hate or Love People like me. we had a good laugh I told her yup that is correct
God Bless the People who care
chil
Thanks, Kathy. I’m experiencing this with a new doctor I went to when I received news of my COPD. I simply wanted a prescription of Xanax to take the edge off. This hit me hard in less than 8 weeks. My pulmanary doctor even recommended it. She’s still refusing. She suggests I seek mental health council.
I understand where you are coming from with the Dr.’s and pain and anxiety meds. I was cut off cold from 7.5 mg of hydrocodone 3x a day after ten years of successful treatment for a chronic condition. I was fully functional and getting checked every three months. This Dr. retired 3 years ago. No one male or female with an MD behind their names will renew my meds, even with a ten year file from that one Dr. They’re just concerned about their future personal riches if their loaned are besmirched.
Cathy, I’ve read people’s comments all the way down to yours and have noticed how lucky you are to be given the pain medication that you are. My husband was 55 when he died of Core Pulmonale but due to my husbands history of drug abuse, the hospital staff were adamant that he shouldn’t be given ANY pain relief as it was detrimental, yet the few times he was given only 5 ml of morphine this helped him immensely and he was comfortable and ALWAYS got a good nights sleep and appeared more stable and happier. I will always resent the hospital staff as he never was a man to complain, such a strong and powerful man reduced to tears from the pain he used to get, makes me look back and wish to God he was given some kind of pain relief because I knew how much pain he was in and it broke my heart that I couldn’t help him. He discharged himself 3 days before he died, saying there was nothing more the hospital staff can do. He invited his sister over to our house the same day and told her, not me, that he knew it was only days until he was to pass. He left the hospital on Monday and died in the early hours of Thursday in his chair. I like to believe he died in his sleep because it was the first nights sleep he’d had in a while and appeared to be in peace when I awoke. I know my post has no medical advice but I’d like to just say, I wish you peace and keep your close ones involved and tell them everything, they’re not mind readers, I know I missed an awful lot whilst caring for my beautiful best friend, he didn’t tell me half of what I wished he had, just so I knew how to make him comfortable, just so I could at least put a smile on his face. I now miss him terribly and 6 months have passed, it feels like I’ve lost him all over again. I wish you the very best Cathy and everyone else who is affected by this ruthless disease, learn as much as possible about it, I wish I had.
I am so happy to hear that there are some Doctors willing to take care of there patients. I’m so happy you have found a place that will let you have the best quality life possible by treating your symptoms. These doctors have no idea what any of us are going thru because they have not experienced it. I’m where you were on the recliner , coughing constantly. Short of breathe, along with buldging discs in my back, arthritis and fibromslgia, depression and major anxiety. You feel so alone in it all and no where to turn. My family can barely stand to be around me because I’m so miserable. I have read where a lot of these drugs are beneficial to us and give us quality of life. Don’t we deserve at least that.
We are suffering !
I’m also labelled drug addict or drug seeker. Stage 4 22% lung function but still relatively ok as I’m quite young., Can’t take cannabis even orally as I’m hoping for transplant / LVRS – was the one thing that made me feel accepting of my situation and made it bearable. Docs happy to stick me on antidepressants though, which I don’t want. The diazepam 2mg, that I take just couple of tablets a week when anxiety is overwhelming, was given to me by a now-retired doc, and the new docs is unhappy with it. Why can’t GPs be educated, he was shocked when I said another transplant hopeful was on lorazepam and oramorph, I shouldn’t have to tell the docs that it is standard practice. They don’t get the suffering we go through. Though I look great when I try to do physical things the suffering starts , 2 or 3 times a day I think this is it I’m going to die, that’s how bad it feels. And the docs is worried about me being addicted to drugs, even though his anti-depressants are just as addictive. (though they don’t call it withdrawal for anti-depressants its “discontinuation syndrome” – the lying hypocrites
My wonderful husband passed away on 24th November this year, in he’s final hours he asked for he’s nebuliser. The windows to be opened, but this was not unusual. He suffered hardest for the last six months and the wasting effect on his poor body was heartbreaking. I fought for everything for him. For he’s oxygen,for the special mattress, even for the forty-juice. It has made me stronger, but angry. I held he’s hand as he smiled at me and took he’s last breath unable to fight no more.he was just 64. I have a family left devastated. It’s one of the most awful diseases to come to terms with,and my love and blessings go out to anyone who is with a loved one trying to fight this disease xxx
Yes I have just been told my husband is the last stage of his copd. And he has an obstruction in his lungs,I asked for oxygen to help him when he has trouble breathing,they said we would have to qualify,do you have any suggestions for me ,I am feeling anxious and under qualified,please help.
the dr can do a simple test called a pft pulmonary function test then insuance, medicare , medicade or a hospice will provide an in home oxygen concentrator a good pulmonary dr will help you get everything you need and answer all your questions
Im dealin with it with my wife she just laying in bed she slept for the last week pretty much all the time
My mother must has been in Hospice since Spring of this year. The Friday after Thanksgiving, she ordered a hospital bed and has declined every day since. She is on morphine every hour and is hallucinating. Her muscles are in atrophy, but she wont take the hand of God and let him take her to heaven. Seeing her suffer may be more difficult than what she is now experiencing. The Dr. said she will “drown” and gasp for air and choke in her final moments. I pray her heart just goes out. If anyone you know smokes, urge them to stop. This is a horrible disease.
I was with my uncle when he died from COPD. He was resting peacefully under sedation and wasn’t drowning, gasping, or choking. I was watching him when he suddenly but quietly lost skin color and peacefully drew his last breath. He had a caring lady physician from Syria who made his last days comfortable with her obviously capable medical skills. Having experienced doctors of widely varying talents over my life, I’m familiar with the less competent ones who can make your life miserable with their inflexible ego-driven attitudes about treatment and medications or their inability to exhibit ordinary compassion that most human beings exhibit naturlally or at least try to exhibit out of respect for the circumstances. I suspect some suffer from mental health conditions themselves that compromise their ability to maintain a tolerable bedside manner. I just wrote this to let people know that, given my uncle’s experience, the end doesn’t necessarily have to be an agonizing experience for the patient or his friends and family when competent care is available.
Have cipd in the final. Stage. May sound dumb but I am ready. God bless
It’s not dumb. You have made piece with yourself.
My aunt is in icu right now in what I now see as probably the final stages of copd with heart failure. I knew she had trouble with her heart, but no one told me it was copd. I went to see her yesterday and I knew she was dying. They have to keep the oxygen mask on her all the time. She won’t allow the respirator. She wants to go home, but how can she? I feel so bad for her, even though I know her smoking is the cause. All I can do is pray..
My mom pass way on the 11 of this month she had copd they haven’t told me why she pass away yet , I don’t understand why the doctors never told us this could happen if u have copd my mom was find her birthday was on the 8 and she was laughing and everything I just don’t understand what happened
I am sorry for your loss. My Mom just passed on February 23rd. She lived with this for several years. But in the end, her heart could not compensate for the lack of oxygen. Medication was futile. She was not as bad as she could have been. Sometimes the heart can just not keep up. It is an awful disease…
My sister is in last stage COPD at 50 years old and she contracted the disease a couple years ago. She has smoked the entire time up to this very moment. Her oxygen mix cannot be increased. Her meds are strong and address all the anticipated symptoms. My step-father was having very bad health and he smoked every minute of the day and would get up at night. He grew tobacco and had a cigarette-making machine. He could manufacture all the cigarettes he could consume. Before smoking could take him away, his smoking caused an explosion that killed him. My mother is in last stage COPD and did not inform me, or let anyone else inform me, until she was hospitalized when all the truth came out. She has smoked all through her treatment. Now, she is confined to a hospital bed while they search for a hospice for her. She smoked all her life..and I begged her all my life to quit. My uncle has COPD. A woman I work with has COPD and carries around her oxygen. I was the only child of four that did not smoke. Both my parents smoked profusely. I lost a brother and will lose my sister and mother. Soon. I am thankful to God I never started smoking and I’m 56 years old now. Getting this disease is like having your forehead immediately stamped with the words
“I am terminal….but don’t know when.” My family has suffered immeasurable damage due to smoking and alcohol. Cigarettes are a curse on mankind and is devastating to the victim, friends and family members. This devastation and things to come are on my mind most of my day. Day after day. One of my best friends lost a sister and a brother to COPD in the last few years.
I have copd and curse the day I started smoking .I am 69 years old ,i do not know how much longer i will live ,i quit smoking when I was 50 and had to retire at 60 ,I am grateful for everyday i have left and try to make the most of it …
Hi sorry to have heard about your situation . I sort of know how you feel not being told . My mum told everyone in my family about her copd 3yrs ago . I found out just today. It felt like a punch in the stomach finding out about copd. But felt 100 times worse to find out everyone else knew 3 yrs ago and kept it from me. How are you coping . Dave
I have copd am on 3rd of oxygen. I use combivent and when i run out of that i have stupid pro-air otherwise if I run out of oxygen body fluids pore out of me.it’s embarrassing peeing my pants and other things. I had a good doctor now I just see doctors in training have asked why this happens and they suggest going to a urologist because they don’t think it has anything to do with copd. I have a good bladder. I have a good heart. I get pain in my left lung and always go to my heart. I have broken lungs with emphysema and asthma. I get depressed a lot I take hooked baths cause any exertion I can’t breathe. I also take care of an paraplegic man in his eightys and it’s getting really hard to do. I am just tired.
My mother in law has been seeing a student OPD Dr for the last 8 years after going to visit with her son in Oklahoma City and having a bad cough attack they took her to the hospital and found out that she has stage 3 lung cancer is there any reason why her pulmonary doctor would not have found this in the eight years he was seeing her if so what can we do about it?
May God Bless all of us with this disease!! I was diagnosed with COPD in 2002 before I had a non-invasive spinal surgery. I didn’t even know what COPD was. All I know from reading all of the comments is that the last few months of my life will be hell, since nobody is really educated about this awful disease. I am very blessed in that I know Jesus as my Lord and Savior and he has far greater plans for me once I leave this earth.
Today I helped my 2 kids pack up their 63 year old Dad’s clothing to donate. He passed 1 week ago ago from COPD. While going through his dresser we found a letter his son wrote him when he was in elementary school. He had watched a video in school that day about the dangers of smoking and all It would do to a human body.he begged him to stop, he didn’t want to watch him in pain as he died. That is exactly what happened. This kid took him to so many doctor appointments trying to get on a transplant list. The last weeks were full of panic attacks and ambulance rides in the middle of the night. Most of the last 2 months were spent in the hospital. That letter written many years ago obviously meant something to him, it was in a dresser drawer right next to his bed. We wish the addiction could of been over come back then, maybe he would be here to see his son get married in April. Now we will have a memorial at his chair. All of you fighting this disease I wish you comfort. Spend as much time as possible with your love ones and say everything you need them to hear and ask them to tell you the things they may be holding inside. The less regrets on both sides will make things easier. May Gods presence be with you all.
My dad died Jan 30 of heart failure due to COPD, he had all the symptoms- but never smoked. He also never told us (4 grown kids) how bad he was. He was very overweight which caused his difficulty in exhaling the co2. I was with him as he passed and will never forget it.
He was heavily sedated with morphine – I just pray every day that he did not suffer because even with the oxygen he was gasping for air,
My mum is last stages COPD, my mum is 63 years old, she is my hero. Mum left side is stroke effected, she has no use of her left arm and has hardly any use of her left leg, last time mum was in ICU the doctor estimated her lung function at 20 percent, that was around 3 months ago, since then mum has made the decision not to go back to hospital, which I respect.
Mum has recently started pernament antibiotics and predisilone, she makes small steps around her unit without oxygen, she weighs around 40kgs if that, she struggles very badly with her breathing, we have been told that she won’t make it through another winter, I’m not sure if I should be looking at hospice support yet, I’m scared of her not being as comfortable as possible. She is the strongest, bravest person I have ever met, I’m feeling the end of life is drawing very near for her, I’m scared for her, what is the best way to support my beautiful mum?
It’s only been a little over a month since I lost my dad and it’s the hardest thing I’ve ever experienced me and my father were close my family and I all knew my dad was not well but no matter what your told your never truly prepared for that day I feel somewhat blind sided because at the hospital no one really says exactly what is going so I think you should get any support ahead of time so that maybe it can make your mom and you both a little more comfortable with the situation I wish now I had a little more support and info for my dad and myself. I truly sorry that you have to go through this I don’t wish this on anyone
Hi Becks, whilst searching for some guidance and support i read your post and can totally relate to your words. I am sorry you too are experiencing seeing a loved one suffer with copd or coad as its now know as. Ive come back today from taking my mum to her gp which was supposed to be a routine visit for a regular vit b12 injection but ended up requesting a gp assess her as her coad was exasperated. I struggle like hell to see mum struggle, she was once so independant,a caring person and so quiet and placid. She is housebound now, used a wheelchair to get her to gp today as shes so frail. It tears me apart to see her suffer and i would love to see her have just one day of comfort. I hate getting upset and know she would hate it if she knew i was upset and i tell myself i have to take this as she is taking much worse by not being able to breathe with ease or do the most basic daily tasks anymore. Terrifies me losing her as shes my rock but i sometimes wish for her sake she passes so she no longer suffers. Ive nursed for over 30 years but this is the hardest thing ive ever done. Sorry to air off here! Just lost and finding things so painful. Carolan x
I’m 35 and just lost my dad on January 28 at the age of 61 he was diagnosed a little over a year ago and it progressed rapidly considering he did not quit smoking I thought my tears and pleading with him would work but smoking had to much of a hold on him he went peacefully but that does not ease the mind of loved ones I will forever replay his death in my head it’s a horrible thing to do go through I quit smoking myself 10 months ago because I do not want to put my children through unnecessary pain. To all suffering from this I’m truly sorry for you
My mother passed on 3/14/15 from COPD. The last 6 months of her life, she was in agony. She had her right lung collapse 2 times within 3 months. Finally, she told me she had had enough on 2/28/15 and was placed into hospice care. She lived 2 weeks. She passed on a Saturday and yhe Thursday before, she wanted to get up and watch Law And Order. We did and ate popcorn and drank hot chocolate. That night she went to sleep and never woke again. She slept until her death 3 days later. Ahe had fallen in August of the previous year and broke her back, however, because of her lungs any surgical option was not possible because she could not be placed under general anesthesia. It’s a horrible disease for the patient and the family. The rapidly approaching anniversary of her death is hitting me hard. I do find peace in knowing that I took the best care of her I could and she was comfortable and did not suffer. I was honored to be her caregiver and consider it to be her final gift to me. For her to trust me enough to provide for her every need and want in her final days was a huge deal for me. To think that she trusted me that much and knew I loved her enough to do it, was enough for me. She was ready to go and I find a lot of peace in knowing that she was not alone. It was so hard to let her go, but a honor to be chosen and be able to be there as she passed. To all suffering from this disease, I wish you peace and all thet love that my mom had in her fin days.
My mom is at the end of COPD and in a Hospice Facility. She just turned 81 on March 20th and on that day she had her “burst of energy “. She knew everything. It was unreal but gave us false hope. It lasted 2 days. My mom was in agony, too. She constantly begged us to help her die. It was horrific and made us feel so helpless. Watching her struggle to breathe and suffer in pain changed my mind about that Doctor who assisted terminally ill patients pass with dignity and end their suffering. Until someone actually experiences it, they truly have no idea how it feels to watch someone you love suffer from COPD. 2 weeks ago Hospice stepped in and it looked as if they could manage her pain & help her breathe easier. We were so relieved. However, after one day, she had what I now know is called, “Terminal Restlessness “. It was like a light switch. She had the strength of a thousand men, screamed for help, started speaking to loved ones that have passed, was severely agitated and very paranoid. She was calling me mom and then tried to punch & kick me. Her vocabulary became unbelievable! I didn’t even know she knew any of the words she was saying and calling her granddaughter. My kids are her world and she’d never speak like that to anyone! Especially her 15 year old granddaughter. She threatened to kill me, accused everyone of stealing, afraid of us and spoke a different language. It was terrifying so I immediately called Hospice. Her pulse oximetry was 70 when they arrived. I forgot to mention that she tried to take her own life a week prior by sabotaging her oxygen machine. She turned it all the way down and messed w/ the tube. It looked like she was getting oxygen but she wasn’t and it was like that for days. She tricked me and I’m carrying tremendous guilt. I should have checked but I never thought she’d actually try to end her own life. I’m probably all over the place because I just got a call from her nurse and my mom aspirtaed. Today is day 20 without any subsequent food or water. Apparently, she may have responded when asked if she wanted yogurt and aspirtaed. I had to look it up. I’m a mess. It’s been 2 weeks of absolute hell. It constantly changes. Hospice has been phenomenal but no one can predict when someone will pass. They said they can only go by how she presents at that time. It’s been a rollercoaster. I have so many questions but my brain is overwhelmed. She was supposed to be moved tomorrow to a end of life facility because she could swallow a little but now, they’re reevaluating her bc she aspirtaed. She’s non responsive tonight. We can’t wake her up. I just wish I had more clarity on this process bc it’s constantly changing. They gave her a week, then it changes to something else. They gave us a book for end of life signs but my mom has gone through almost every single one down to days left. Is aspirating a sign that she’s declining? I’m sorry for the extensive message but we are literally going through this right now. I need help understanding all that’s happening and hope and pray that someone can offer some guidance so we can be prepared. I don’t know what to do!!!! Please, if anyone can tell us what’s going on, we’d be very grateful. Thank you for reading and for sharing all of your stories of your loved ones. I didn’t even know that she had COPD until 2 weeks ago. I thought she just smoked too much and had bronchitis. The guilt is as heavy on my heart as her suffering is. God Bless all of you and those affected by this horrible disease.
God bless you Sweetheart. I wish you were my child. I am close to my hour of death. My daughter totally abandoned me after financially exploiting me and a lifetime of emotional abuse. I accept, but my heart is splintered. No one will be holding my hand. But soon my God will wipe away my tears. I am 73 – amazing with all the deceased I have endured. COPD is the worse.
God bless you all .My mother has had this desease for a long time now has chf hep c degenerate boon desease internal defibrillator for the last four months and has been on 24 hr oxygen 2 LTS. For about a year but we just took her in the other nite she stayed 2 nites we found out she had level of 74 of c02 in her blood blood pressure was 212/77 sugar was 315 diebetic BTW they ran a bi-pap for about an hour and the next day ran another test level was 66 every Dr has said she is at the last stage of every desease the dr at the hospital wanted to run more test and told me the results would only change her care with blood thinners she wanted to come home we decided (her and i) to check her out and bring her home got her here last nite I have hospice coming on Friday any words of advice would help thank you and God bless
Tony Perrotta Colfax CA
This is crazy…absolutely the most devastating thing about life is watching my mom suffer from COPD. She is in ICU rite now and it hurts like crazy to see her on the ventilator. I pleaded with her about 10 yrs ago to stop but she is grown and will make her own decisions. When her COPD got worst I moved with her to care for her. One night she was breathing funny and couldn’t keep a steady pace of breaths. I called 911 and ever since then she has been in the critical care unit on a ventilator. I don’t even kno wat to expect not to pray about. I kno she is tired and it just hurts so bad to see her like this . I educated myself but I’m just not ready to let go. Idk wat to do
I can completely relate and while we have been dealing with COPD for 10 years, my mom finally passed on 3/26/16 and it was so hard to let her go but it was something she wanted. She has reinstated the DNR on Thurs as we didn’t want to see her vented again, nor did she. Sending prayers to you and your mom. My heart is hurting so much!
My dad passed away two weeks ago with copd and core pulminore me and my brothers and sisters sat with him that night and I will never forget the noises of panic and choking that my dad made. I couldn’t bear to c it too the end and left an hour before he died this will haunt me for the rest of my days I’ve gave up cigarettes as I swear my children will never have to witness their parent die in such a horrific way I loved my dad and always will he was my hero and always will be.
Was looking for answers and came across this article. It was so very helpful. Than you. I am currently care giver for my mother who is in severe end stage COPD. You would think I would know this stuff because you see I am a primary care Physician Assistant. Most of it yes I do know (diagnosis, treatment of exacerbation and starting oxygen therapy). The hard part of course is the not knowing which is why I am searching. For example when to let Hospice know she is to the point of needing Morphine (because all logical medical sense tells you Morphine suppresses respiratory drive). It is such a fine line between doing what you are trained to do (which is “do no harm”) and doing what needs to be done. AND between being a daughter and knowing what’s to come. Thank you for providing just the right guidance my heart needed.
What is really amazing about this article is that it still makes the “Most Read List” after being posted almost 7 years ago! End of Life issues for COPD hit a very responsive chord. As a Respiratory Therapist I have worked with our local inpatient/homecare hospice for over 10 years. The opportunity for RT’s to provide palliative care are unending.
I witnessed just last night the calming effect that a properly fit PAP mask had on a very frail man in the final stages of CHF/COPD. The mask he came with from the hospital to the inpatient hospice facility was too large causing leaks and subsequent discomfort and agitation. The correct mask was calming and soothing – Helped him and the family. A small thing? I think not.
Pay attention, Be Kind, Help Out – It costs little – Means Much !
Please read my reply to another post below. I need help understanding what’s happening right now. My moms nurse just called and said my mom aspirtaed.
Thank you in advance.
My husband is 62 and in the last stage of COPD. He was in ICU in December 2012 with type 2 respiratory failure and has not smoked since then, if only he had given up years before when first diagnosed. He is having palliative care now. What I find so hard is the not knowing when the end will be, I don’t wish him dead but I don’t know how much longer I can go on with this hanging over us, He gets so nasty verbally and so angry, I cannot do a thing right. The man I married is long gone and I am left with someone I would not choose to stay around if I had a choice. Its sooo hard, I am grieving yet my ‘husband’ is still here! sorry if that sounds harsh but we are both struggling.
You are not alone.
My father is 65. He is also in end stage COPD. He has been waiting for a transplant for four years. He is too weak now to receive the transplant and has been taken off the list. He is mean and angry towards my mom and is so depressed. It is so hard to watch him suffer for so long. My prayers are with you also!
Susan, my father in law has COPD but refuses to tell any of us what stage he is in…after 4 stays in the ICU in less than 6 months, my husband and I decided to have his parents come live with us because we weren’t sure how much time he had left. That turned into a huge mistake because he is so verbally abusive toward everyone and unfortunately it’s not just the COPD/ asthma, he is an alcoholic, kidneys are only work at 40%, diabetic with an enlarged heart/CHF oh and did mention his noncompliance!! We all love him but he makes everyone miserable because of all his health issues, he is completely capable of taking care of himself but refuses to left a finger unless it has a beer in his hand! He will intentionally say things to hurt people and openly admit it, will give anyone a silent treatment just for fun but mostly keeps pushing the people in his life that care/love him further and further away. I understand your pain and wondering when it will all be over because as I tell my husband, it would be easier to grieve for him if he has passed away then to spend however long he has left grieving for the man we used to know!! My sincere condolences to you and your family, stay strong and remember to take care of youself!!!!
You are not alone! My father is in end stages and is so angry. He’s quite old (86) and is also showing signs of dementia. I am already grieving the father that’s gone. I wonder ow long he will live in this terrible state. If he was more alert he would choose to end his life but his wife is selfishly choosing life prolonging measures. It’s one of the most terrible experiences of my adult life. A horrible way to see your parent. I’m so sorry for you. I understand how you feel…
I have never seen a disease, not cancer, nor AIDS that is written about with the most dramatic, overtly negative words. It’s disgusting. If, they didn’t put so many diseases under 4 initials it would be different. Come on there are so many people in the world diagnosed under those same 4 intials. Everyone over the age of 40 has diminished lung capacity. That’s a fact. But, this disease is a stock portfolio holders dream. It’s got to stop. Instead of writing another horror study, write something innovated on researchers and hope.
Until you loss someone like I just did last week to COPD (Chronic Obstructive Pulmonary Disease….does that sound better tom you?) shut up! What do you know. This disease robbed me of my husband of 29 years and our three sons of a father. Do not post what you clearly do not understand. You are a very insensitive person!
I am sorry you do not understand what these patients and families go thru with COPD, but you should be thankful you have not experienced it first or second hand. It is a torturous death, like drowning or suffocating over yrs. Please do not judge others on something you obviously know nothing about, and show some empathy for others suffering, or as our mothers have always told us, don’t say anything if you can’t say something nice! I have been a respiratory therapist for over 30 yrs and have watched many good and wonderful people suffer a slow and agonizing death. I would not wish it on anyone!
Lost my sweet mother March 8, 2016. She was diagnosis with COPD many years ago (maybe 10 yrs). Heavy smoker for 50 yrs, but quit with diagnosis. She had very little trouble with COPD and no doctor seemed overly concerned by her diagnosis (she did have vascular diseases, most likely due to smoking). She never needed oxygen, nor inhalers, then suddenly she plummeted. She went into the hospital with chest pain and didn’t leave. She passed away 3 wks later. Death certificate reads chronic copd, pulmonary fibrosis and respiratory failure. I feel blessed to have shared my life with her for 55 yrs and 3 days, but my heart still aches. She was 76 yrs young. Love and miss you momma.
Hi Lor Ray,
I am so sorry that you lost your mother. You were very lucky to be so close with her and she was the luckiest to have such a loving child.
i am 24 and i have pretty bad copd i am on the highest dose of the breo blister inhailer 200mcg/25 that i take once aday and so far it is amazing i started out on the 100mcg/25 but i found myself no being able to breath and in a panic after 12 hours having no choice but to double dose, does this mean i am more progressed then most ive gotten alot worse in the last weeks and im having serious memory problems, i drove 30 mins to what i thought was my job site that i just worked at the day before to realize i was driving to my friends house, this is absolutly terrifies me. my muscles they burn so bad i cant do anything without loosing my breath. my lungs burn with every breath does anyone else have this burning all over their body like you just worked out all day litterly i cant even pick up a fork sometimes it just falls right back to the plate im just so damn tired
I will pray for you
Christopher, you have way more than just COPD going on, get back to your doctor, or find another one right away and get them to figure out what all is going on with you!! I have been a respiratory therapist for over 30 yrs, no one at 24 has all what you have going on due to simple COPD. I will be praying for you, but you need to find help immediately!
I lost my father to copd and now I’m losing my father in law to it as well. My father didn’t quit smoking but my father in law did 40 years ago. I can’t help but wonder if those that are saying their loved one was mean and nasty at the end of their days did your loved one take prednisone, because that one of the side effects as well as deterioration of the bones if token for a long period of time.
My husband of almost 29 years just died last week of end stage copd. The hospice nurses gave us these crummy book detailing everything to look for, but my husband never followed or showed the signs it talked about. I wish the doctors had been more willing to be honest with us on how long he actually had. He struggled in pain for 5 years. Doctors are so worried about getting sued these days. His would not even talk to him. Such a dis-service to end of life patience’s. The hospice nurse was not any different. Makes me so angry all the while I am battling my grief.
I lost my husband of 35 years to end stage copd. He passed away on 05-20-16. We had to put him in the nursing home. He was in there a week and they put him on hospice and he passed away 2 days later. He was in a lot of pain. He got where he would not eat or drink anything and he was very weak. All he would say was I am ready to go to my heavenly home. It was hard to let go and it is still hard on me. I truly miss him. But I do know he has no more pain. It was so hard to see him suffering like he did. He lost down to 110 pounds. It hurts to know there was nothing more I could do. He was by himself when he passed. They did not think he would go so quick and tears me up to know I was not by his side. He suffered with it for years and he was only 62.
.
My heart goes out to all of you have have posted and to all of you copying with such difficulty.
My dad is pretty sick in te end stages of COPD, he is in remission of liver and Lung cancer, yet the radiotherapy has damaged his lungs. He is on 4/5 litres of O2 a day, he has been told to stay on his 30gm daily does of steroid tablets, this has been increased to 40mg a day this morning via pare medic and GP decision. My dad was informed last week that he is starting to lose his eye sight due to steroids but he simply would have no quality of life without taking them. My mum is his full time carer and she has done an amazing job and still does but her depression has got so bad she is sleeping all te hrs she can 20 out of 24 a day. It is getting to the point that me and my siblings are unsure if my mum can realistically manage his care to its full potential but we’re so scared about trying to discuss this with them without upsetting them massively. My dad has had a continual chest/ throat infection for over a month, he has been admitted to hospital 3 times already this year. His legs are swallen and he can barley get his shoes on. He has started to wet himself, he is often confused and unable to say what he means, his anxiety is currently through the roof. I tired to help out today but it’s so hard it is completly draining. He has started to make a new exaggerated sound when trying to get his breath. He is only able to walk a few steps at the moment without it taking all his O2 and energy. He has fallen over a few times and yet still insists on going up stairs to his bed. Today was the first day he let me support him to walk up the stairs. He seems to have gone down hill week by week in the last month. I have this awful feeling that he maybe coming to his true end. The not knowing is unbarable and debilitating. He discribed his oxygen cable as his green noose today :/ and told me go when his dad died he felt his energy move into him. I just wish I knew how long he had so I knew weather to take some time off work or not. I have been incredably anxious on and off the past 3 days, I can’t seem to sleep more than 4/5 hours at a time, which is rough on my 11hour days at work. Me and my dad are so close and it’s incredibly tough. My whole family are being so brave, my dad is the bravest of us all, he never complains. I can only hope one day I will be as strong as him. I just want to say thank you for taking the time to read and share this. My thoughts go out to all of you struggling with this first or second hand. Thank my lucky stars for good friends, my dog, nature, music and the occasional laugh as without these things I feel I would have broken down completely. Xx
NOT TO WORRY RUTH, I ALSO HAVE THE C O P D BUG, AND SEEM TO HAVE THE SAME QUALITY OF LIFE YOUR DAD HAS. I HAVE A DAUGHTER, WHOM I AND SHE ARE OH SO VERY CLOSE, I LIVE IN N. C., SHE LIVES IN ORLANDO FLA ! SHE MARRIED 5yr AGO,AND MOVED THERE WITH HER HUSBAND. SHE ALWAYS SAID SHE FELT LIKE SHE ABANDONED ME. SIMPLY BECAUSE FROM FEBUARY OF 2008 -2012 I WAS IN,& OUT OF THREE DIFFERENT HOSPITALS WITH A ASSORTMENT OF DIFFERENT PROJECTS. C O P D CAME ALONG DURING THIS TIME. KNOWING THAT GOD DOES NEED EXAMPLES FOR YOU, and OTHERS TO SEE THAT HE IS STILL IN THE MIRACLE BUSINESS. WE, YOUR DAD,& I both HAVE HAD A LOT OF EXPERIENCE HANGING AROUND DOCTORS OFFICES,& HOSPITALS. WE READ ALL THE CERTIFICATES ON THEIR WALLS. EVERY ONE OF THEM STATE THAT THEY HAVE A LICENCE TO PRACTICE ! WELL SOMETIMES THEY WIN, and SOMETIMES THEY LOOSE !! YOUR DAD AND I BOTH KNOW THAT GOD NEVER LOOSES. WHAT MAKES US HAPPY IS KNOWING SOME DAY, WE WILL BE WITH YOU. WE WILL HAVE A NEW EXISTENCE. NO SADNESS, NO SORROW, NO TROUBLES. HOPE I DIDNT BORE YOU, BUT MY FAVORITE SONG IN CHURCH is BECAUSE HE LIVES, I CAN FACE TOMORROW.
I’ve watched COPD take my father and Fibrosis of the lungs take my mother. It was so hard to know and see how they suffered. Most people don’t understand what one goes thru. It’s like someone having there hands around your neck and at times your fighting to breathe.
What would be your reaction? You would panic, have anxiety and angry because no one understands.
I am 58 years old I have been fighting breathing, bronchitis , pnuemonia , chronic sinisitis off and on my whole life. I can say what normal really is. I now have fibrosis and COPD .. There testing for cystic fibrosis I guess a few of us made it thru this far which truely is a mirecle. My quality of life has gone done so bad and I feel hopeless most of the time. I try to stay strong for my family, kids and grandkids but they don’t understand.
We take being able to breathe normal for granite so only those that are there can relate. I pray for each and everyone of you and I want you to know I do understand what your going thru. God bless you
My mom is in her final stage of copd and has been on hospice for 4 months now and i am her main care giver in my home. about a month and half ago she had all the near death signs. Hospice said that she may make it 2 wks and I didn;t think she make it a week. Then one day she woke up starving to death and has been going since. But she is a roller coaster. Watching her suffer daily is so heart breaking.
I don’t know how much longer she has but I pray Jesus takes her home soon as much as it will hurt letting her go, it hurts even more watching her suffer. I am constantly googling copd sites just for some kind of encouragement and especially understanding. Everyday i pray for God to either miraculously heal her or take her home. Every comment on here i can truly relate to and thank each and everyone of you. May God bless you and your loved ones. Cherish every moment you get with your loved ones cause we are not promised tomorrow,
Renee, you and your mom will be in my prayers! I have been a respiratory therapist for over 30 yrs and have watched and waited with many pts and their families as the go thru the last days. It is terrible what they have to go thru and I pray for each and every one. I know you don’t want to lose your mom but that you understand and want her suffering to end is a blessing to you both. I have seen way too many families who won’t let go when they need to. God bless your mom, you and all your family. You will all be together again someday and there will be no more pain or suffering!!
Thank you, since this my mom is getting very little air in lungs and is disorientated Again. Its the watching her suffer that so hard. Hospice said they don’t believe she will rally out of this one. You being a respiratory therapist. When they are getting little air in lungs does this mean their lungs are closing? Her appetite is great. she sleeps most of day but always wakes up starving. is this normal?
I am just confused and just don’t want her to suffer anymore. as much as i will miss her i just pray for Jesus to take her home.
Your story really touched my heart, just wondering how your mom is doing? My mom has copd as well and the doctors say that she is in her last stages and she is in hospice care also.
Rhonda, my mom is still hanging on barely. Its a down hill roller coaster. Been up all night with her. oxygen level has dropped and pulse is in 100. Rhonda this is very hard to watch i pray you are strong enough to care for her 24/7. I am so mentally physically and spiritualy drained. There will be days where she does real good then there are days where you dont think she will make it another day. Cherish the good days and be prepared for the bad cause they are so heart breaking. I will keep you and your mom and family in my prayers. If you need someone to talk to just send me and email [email protected] Believe me having someone who has been there helps a lot. I have done so much research on this disease i could probably be a respiratory therapist.. lol
But one thing i have learned is every death is unique.
God bless you
My God, I am going through the same thing. My heart goes out to you. A roller coaster ride that never seems to end. We thought we lost mom about 4 times now, only for her to rally – causing even more stress and burden. I love my mom dearly but I’d rather see God call her home than to endure watching her suffer. She’s blind, can’t walk, can’t raise a glass of water to her mouth without being winded, COPD, CHF, emphysema and she’s 89. Please pray for us as I will you.
Jim yes my prayers are with you. Its the hardest thing I have ever experienced. She is definitely unique. We are on the down hill ride as of now but i never know she may rally back up again. yet she showing end signs of decreased urine and tea color as well as big decreased in appetite and disorientation. She struggles more to just breath. heart breaking cause there is nothing i can do except to keep giving morphine. I can’t imagine how she feels. Imagine feeling like your suffocating 24/7. Praying Jesus takes her suffering and brings her home soon.
I am trying to figure out the exact things to look for in determining how long my mother (age 58, stage 4 COPD, FEV 23) has to live. She and my father just stayed with me for a couple of weeks while they looked for a house to move back to Nashville from Florida to be around family more.
She is on Oxygen 24 hours per day, steroids, inhalers, you name it. AND SHE STILL SMOKES! However, this last day or two she has gone downhill and hasn’t smoked as much and not at all today. Her oxygen was in the low 70s this morning. Through breathing treatments, inhalers and oxygen we were able to get her back up to the 80s this afternoon. Her toes are purple. When she sleeps you can tell how hard it is to breathe. And, she literally looks like a Skelton with skin.
My dad decided to take her back to Florida today to try and escape the ragweed that is blooming here in TN as we are all allergic. My mom has mentioned twice this week that she thought she was near the end.
Her doctor now refuses to see her since she won’t stop smoking and she is the most stubborn woman in the world, blaming her disease on anything BUT smoking all of her life. She also refuses hospital care since she will not and never has let anyone tell her what she has to do or that she can’t smoke.
I am debating on trying to scare her into allowing being admitted to the hospital or call in “hospice”. I’m wondering if just using that word will scare her enough for hospital care, but what good is it going to be at this point? I fear she is really near the end. Opinions?
It’s time to call hospice, not out of fear but because you need help.
I know how you feel. My grandma passed away last week from copd and she was the same all she wanted was a cigarette. If she was fit enough we’d have taken her for one last one. It’s an awful disease. Hope your mother doesn’t suffer like my poor grandma did. She knew she was dying and she said she wasn’t scared she was just sad! Watching someone you love suffer like that is horrific
My heart goes out to you. I am experiencing the same thing only my mom is 89, smoked her entire life, has late stage heart disease, COPD, emphysema and has caused many roller coaster rides into hell with being in and out of hospitals. She’s in hospice now but refuses to let go. She’s blind, can’t walk a foot without being winded and it’s HEARTBREAKING. She still denies it was the 3 pack a day habit for 75+ years. This situation is tearing our family and my new marriage apart as mom expects our lives to revolve around her. She wants to come home after a 5 day hospice respite and I am TERRIFIED. I am her primary caregiver and completely incapable of dealing with it emotionally and physically. We are all paying for her smoking habit and a heart that was fixed 20 years ago with a titanium mitral valve replacement. Please pray for us, as I will you.
great group all human if you were not praying before for them you should be now
I found this website by accident. I guess I’m used to looking at COPd patients from a professional point of view.
My father, who is currently 81, is experiencing final stages of copd. I work full time and cannot comply with his wishes to move in with me.
My father has been very angry, mean and demanding. Nothing would have prepared me and my siblings for this behavior.
He can de delusionail and accusatory at times.
Sometimes he get tearful. I try not to take this actions personally, but I have feelings too.
He’s currently in a hospice program… those nurses and staff of Intrepid have been very supportive.
I know at some point, when he is actively dying, I want to bring him home with me, but meanwhile, our family will try to support him as best we can.
Families don’t allow Guilt to haunt you. Don’t allow emotions to cause you to make decisions that accommodate your love one, but make your life miserable.
Take care of your self. Visit and support your loved one as much as you.can… and pray to God that he gives you the strength to endure this portion of the journey
Hello everyone. I have been incredibly moved by all of your experiences. My mom is 68 and it appears her lung disease is very advanced. She has interstitial lung disease pulmonary fibrosis and pulmonary hypertension. She has suffered terribly over the last 3 years. In the at year she has spent more than 6 months in hospital. This time is different, she is confused and disoriented. Her weight has plummeted and her sats are in the 70s. She is nit mobile at all as her breathing is so bad. She doesn’t know where she is and is hallucinating. She has been offered hospice care but is terrified and begging to come home. I am truly heartbroken watching her suffer like this for so long. My heart goes out to everyone with a lung condition and I Wi pray fothat a miracle for us all xx
My Dad is in the end stages of COPD. He has truly been such a fighter and has literally shocked he’ll out of doctors! Not only does he have stage 4 COPD but in the last 6 mos he’s been diagnosed with 2 different strains of non tuberculosis micro bacterium infections in his lungs. They are incurable. He’s not himself anymore… my parents are giving up hope and feeling so discouraged that nothing can help him. He’s 70… wonderful marriage of 47 years, 4 daughters, 8 grandchildren. Close knit family. I’m truly scared for the end
My partner has copd got really bad since June this year been of work sick since June infection that just won’t clear up he almost 7half. Stone in weight unable to get to the bathroom without panic breathing his work 20 years not been good with us at all only pay him basic sick pay I’m working my 20hours week coming home take care off my partner. We fall behind on rent council tax we have no family to offer help. I just don’t no what to do for best only 39 years old trying to stay positive don’t no wether this is the end his family thinks he just needs to man up get back to work they visited once in 6months I cannot make them understand what copd does to a person mind and body until u live with it u never no. Feel very worried don’t no how to keep us in our home
So sorry for the stress you are under. Have you looked into getting disability for your partner? It’s a long process but might be a way to get you the additional income to stay in your home. I think sometimes they will have it retroactive to the time that the patient was unable to work.
My mom is in the final stages of COPD I think?? I hate to sound heartless, but some days I sadly, think she is trying to make her condition seem worse than it is. It was the hardest thing I did, but she convinced my daughter and I it was the end for her. Now she expects me to do everything for her. I was hoping to create some good memories with her as I never really lived with her even as a child; I was in boarding school at the age of eleven. Her first condition is narcissistic personality disorder and her COPD is secondary to me now. She is the most demanding person I’ve ever know and every caregiver that has worked for her quits or threatens too. I’m not sure how much I can take! She’s irrational, demanding and has the awdasity to say she will not go to a nursing because “she’s somebody.” How long does this last because I may have to commit myself to get away from her.
Wow. I feel like our mothers might be long lost twins. My mother has OCD, anxiety and a very narcissistic personality. Everything has always been about her. She also has had a drug problem my entire life. She has end stage, and she has been very demanding. Trying to guilt me and my father for not doing more for her. I don’t think she is exaggerating her symptoms, because this disease is terrible and one of the worst ways you can go, but some days I second guess myself. I have a lot of anger that I’m trying to let go. I think the anger is holding me together and it’s only a matter of time before I fall apart. create boundaries for yourself. Mom wanted me to call her every day and see her every weekend but I have a busy job and life and some days it’s too hard. Now I call when I can and ignore her digs. I feel for you. Hang in there.
It seems you did inherit the lack of empathy gene from your mother. It goes with being a narcissistic person. Can you not show some compassion for your own mother, she may be not be what you expected of a mother, but she is still your mother. I lost my own when I was 10 years old to breast cancer…non smoker..a true lady and a great mom.Did you ever think one day your own daughter may feel the same way about you? Things happen, people and children change. You are being harsh on your mother who is already dealing with the most unkind disease…not breathing is the worst feeling on earth.
Hi Lara, my mother was the same as u described. Although my mother had scleroderma she died Nov 1 2016 from COPD. I wasn’t ready to watch my mom suffer for 3 weeks and watch the ordeal go down the way it did. For about a month I watched my mother suffer in ICU. I wasn’t ready for the part when the oxygen to the brain becomes deficient and she no longer knew where she was or what had happened to her. She was more pleasant on the ventilator when she couldn’t talk then when they took her off of it. No one told me my loved one would suffer in pain yelling help help for 3 weeks not being able to breath. I felt like I just had the most horrific event happen in my life. No matter how you prepare your mental well being is never ready.
Do you have access to inpatient or outpatient hospice services? Sometimes there is a hospice house (better for most than a nursing home) where she could get 24/7 care. Hospice would also give YOU some help with coping mechanisms, support etc. Hoping you can get the help that you both need. Take Care
Well you are a better woman than I because if I didnt love her very much no way would I take care of her. It doesnt sound like when you were a child she was there for you. Only way anyone can tell how long is by what the doctors say and they are never sure. I would pull them to the side and ask how long they think. I would let her know if she doesnt quit being so demanding you are going to have to put her in a home. If she is in last stage of copd call in hospice to help some. No one can judge you unless they have been through same ordeal as you.
Wow I read this and wondered does anyone actually get what your going through . I am in that same position ,your not alone. My mom is narrsastic and demanding and manipulative . I pray every day for the end of this yet I keep my thoughts within myself. What this has done to me ,I cannot describe. .i have so many bad thoughts I wish I could control .guess I’m just looking for that way out. There is got to be a time that you decide to walk away and live. I am. To connected to a tube or a machine but my mom has made it like that for me
I’m at end stage with COPD as horrific as it is going to be I’m so thankful I found this website. Not getting any straight answers from pulmologist and evasive when I ask question regarding palliative care. I struggle every day and feel so alone because no one seems to understand what I go thru. The medicine that would make my breathing a little easier is denied by my insurance. The 5mg of opiate I can’t take, because I’m treated like a drug addict if I take it daily. I struggle daily, my life is based on how far I can go without my oxygen. These comments helped me understand what I am to face while my heart hurts for the survivors. Although no one in my family understands in a way I’m happy because when it gets really bad they won’t know. That’s what parents do we protect. Don’t be mad at us, be mad at a world that allowed this poison into the world all for the mighty dollar.
I just notice someone saying “It seems you did inherit the lack of empathy gene”. Then she goes on to say what a great mother she had. I never believe because some one is a blood relative you love them even though they treat you like crap. If she walked in your shoes I am sure she would shut her mouth and not be so judgmental. Just treat your daughter with love and not send her to boarding schools and she will be there for you when you are older.
believe me they know what you’re going through this is what pisses me off about a lot of doctors and specialistthe reason I know this is because my wife is in COPD stage 4 final stage and is suffering immensely I’m watching her deteriorate everyday it’s very sadI wish you the best of luck and may God be with you
My husband was told he doesnt have long to live. ( six months). He is 71 and has be in the hospital three times this year. He goes in for like a week or two then back home. He does really well and doesnt seem to be suffering much. I honestly believe he would be dead by now but a year and half ago doctors wrote prescription for a non- evasive ventiltor. It is called Triligy and the doctors actually tell me to bring it up when he is in the hospital because it is better than what they have. I get it through Lincare. He has been on 6 liters of oxygen for 2 years. He takes two nebulizers in morning and two at night. The the fast acting three times a day. He is on 10mg of predizone unless he has low oxygen levels then doctors up it. Since he is on the ventilators 12 to 14 hours a day his levels read between 88 to 93 usually. He hasnt been about to walk more than one step to get into his Hoveround now for 2 years. He gets up once a day for bowl movement sometimes less because he is on morphine. It tends to cause constipation. Doctors prescribe 15 mg of long lasting morphine in morning and at night then 15 short acting as needed. He chained smoked for 52 years I begged him to stop but he never did. Now he is paying for it so I dont say I told you so. I am paying now for him being a chain smoker. I stopped smoking when I got pregnant with our child. I didnt allow him to smoke in house after our child was born. So that helped his habit some. Problem is my health is bad now and I am in a lot of pain. He cant walk so I have to take care of him full time with no relief. Also like many people on here are saying our love ones can be demanding and inconsiderate. So what was suppose to be our golden years have turned into our suffering years. I do my best to make him happy and make him anything he wants to eat. I just hope his heart goes before he really starts suffering. I seen on her someone said their loved one was screaming Help help in the hospital for 3 weeks before he died. I just doesnt understand this because my doctors told me they wouldnt let him suffer they would knock him out with strong meds so he wouldnt feel a thing. I hope this is true I couldnt take seeing him suffer bad.
I just seen where a women said her mother tried to kill herself by shutting off oxygen. If she is suffering why would you stop her??? My husband was offered in hospital to end it for him. They said if you want to go let us know we will make you comfortable and you will die. I know if I was suffering I would want to go. I have told my daughter this.
I re read this article…#1 this very old 14th century disease, should have been cured centuries ago. GREED, and GREED only keeps as the author states this devastating disease uncured..why the person writing this a RT…making money off of pulmonary patients.Yet, will write that the person dying should be treated with “respect”…WOW. People, all people involved with COPD have remained too complancent…write letters to your Congress persons, Senators, federal and state…let’s get this disease cured…and cured fast…it’s cure has been put off way too long…let’s pray the 21st Century Cure Act cures…COPD…and it’s not just smokers disease anymore…..
The cure is to stop smoking before too late. I dont believe there will ever be a cure for copd. If you smoke and turn your lungs to a hard black slab of meat dont expect there ever to be a cure.
I was diagnosed with COPD at 37 years old. I never smoked. My dad did but I only lived with him through high school years. So what’s my excuse?
Hi, I am a 65 year old woman as December 11th. I was diagnosed with COPD ten years ago. I have been in and out of the hospital with exacerbations 11 times within 12 months. The doctors than put me on hospice, and I was on it for a year, and decided it did not benefit me. My only concern now is the weight loss. I lost 60 lbs in 7 months without trying. Other than that I am not depending on O2 except for during exertion. I am taking care of two young grand daughters ages 14 months and 5 months which I enjoy doing. They have given me the power to fight, not saying I am perfect, I have my good and bad days. I was wondering if the weight loss is part of the end. Does anybody have any insight??
Sincerely awaiting your response
I would strongly suggest you see a Dietician. Proper eating with a COPD diagnosis can help you thrive. The right balance of proteins and carbs will give you the energy you need to breathe. With COPD you use a tremendous amount of energy to breathe. Much more than someone with healthy lungs. This is why significant weight loss is very common among those with advanced COPD. As a respiratory therapist, I see this happen all the time. I hope this helps, Sarah!
I cant believe you arent on oxygen full time. What does your oxygen read during day?? The weight loss should be something your doctor should be very concerned about have you talk to you doctor about this?
I wish I had more time to spend with you tonight.I to, am in stage 4 COPD 24/7 oxygen. I feel like a prisionier because ecev walking to my car to go pick up my prescriptions scares me. Plz get back on one day so we can talk.
I am 61 years old and am facing end stage COPD on my own.. I live 10 miles away from my small ND> community and am becoming increasing more fearful of being on my own. My weight has dropped to 120 and my muscle mass and strength are near non-existent. Getting anywhere is difficult as this winter we have had more than 54 inches of snow.
I know it is wrong, but if someone could help quietly end my life I would be so grateful .. I do not have a spouse or children and depend on a cleaning lady who is kind and good, but I can only afford her services every other week.
I have had a wonderful life of education, experienced a great love affair, studied and traveled abroad and seen wonderful places and people. A family of people who have loved me deeply and a faith of hope and joy with my Creator that has been with me the whole of my life.
For that past ten years I had the privilege of assisting and caring for my elderly parents. My father died of COPD and the last 72 hours of his life were intolerable to watch. He suffered so. Then this past August my mom passed away from a rear cancer that spread to here lungs, her brain and stomach. Her struggle lasted just over 30days. Her relationship with her children, her siblings, her faith community and her God let her pass with great dignity. Sadly she suffered her entire adult life with debilitating Asthma – yet she achieved so much.
I don’t know why I am sharing all this – perhaps because I don’t want a long struggle and horrid pain at the end and wish there was a resource to end my life without great expense to society and would provide my a gentle transition from this life to the next. S many resources &information on the Web but nothing for this kind of assistance.
z Mitchel peace be with those who suffer.
<3
God bless you Russ, thanks for sharing your feelings and nice life stories and happy memories of your life with us. You are in my prayers X
God Bless you !
Can hospice help you? My prayers are with you.
My mom is in the same place as you. I am so sorry to hear. She asks to leave the earth and her suffering everyday. I wish I had an answer but I do not. You are in my thoughts and prayers. God does all things for good! He will take you home peacefully when he is ready.
It breaks my heart hearing your story Russ along with all the others. I just lost my precious mama to this terrible disease this past Friday. You have to put your trust in the good Lord to carry you through this. He is our only hope no matter what we are facing in this life. My prayers are with you and many others that are battling this. May his strength and mercy cover you
Exit bags are quick and painless. I too have watched family members go quite painfully. I believe that god forbids suicide as he does not want us to waste the precious gift that he has given us. But with COPD, it’s the choice between jumping out of the window of a burning building or turning and walking into the flames. There is no point in living if you have no quality of life. I truly believe in that.
I’m also in endstage COPD. Right now, I still have about 70% good days but that is starting to change. Soon, I will have to relieve myself of this burden and move on. I hope that someday, we grow up enough as a society not to have to starve our loved ones to death because we’re too afraid to be the hand that pulls the plug.
Thank u for
I lost my dad last week to copd. He smoked for 60 years a pack a day. He suffered a series of strokes 2 years ago and had stents put in his neck weeks later. The strokes gradually brought on dementia, that with his breathing also brought on tons of anxiety and confusion.
Ambulances and hospital stays, specialists, puffers, steriods, antisychotics, pain management, oxygen, nursing homes, full care residents and drs always messing with doses cause they could never seem to get it right. Hallucinations. he gradually never knew where he was or who anyone around him was except my brother and I. I’d walk in and see him looking confused and anxious then he’d see me and it was like everything was like it was before. Hey son he’d say, where have you been?
It was the roughest time of my life I thought, until now. Cherish these final moments people, it comes quick. You think you have time.
I also have COPD. I have looked into Right to die states. You can get more information by googling right to die states.The states that allow you to die are:
California.
Colorado.
District of Columbia.
Oregon.
Vermont.
Washington.
John im scared im caring for my dad at hime. He is off all regulat meds.just dilaudid drops and ativan to make him comfortable. One minute He says hes ready and to.dose him up and knock him out and next mi ute he says he wants to stay with his girls.im so.co fused and scared of hiw this will all go.
My mum is 59 yrs stage 4 copd, emphazema, lewy bodies dimentia, alomg with numerous other health conditions. She has had multiple TIAs and had a stroke a few momths back. They diagnosed her with stage 4 copd 4 1/2 years ago. In December we were told she had only 30% lung function. 9 days ago she was admitted for pneumonia. Within 3 days it was cleared up. She continued to go into respiratory failure. They wanted her to go into a rehab facility for 2 weeks and in her living will it states not facilities for any reason. Me being her power of attorney i must obey her wishes. So today we finally got to bring her home. Now her doctor at the hospital was completely against it and never consulted me about her care even though mom has hallucinations and is confused most of the time. She knows where she is but continues talking to people who aren’t there. She cant see them but hears them all the time. Needless to say i am not pleased at all with her care she recieved as far as consulting with myself. Ive cares for hwr since ahe got sick. I auit my job and dedicated myself to her. I have a husband and 3 sons 13,8,21 months. All the doctor would say to me is she has less lung function than she had in december which was 30% and she needs a rehab facility and its her copd and emphazema. When i brought her home(which she recieves 24/7 care i might add) i read her discharge papers and it stated chronic respiratory failure…. now my question is how long might mum have. I wanna give her the best quality of life that she has left. She wont take hospice but will take home nursing for physical and occupational therapy. Im the only one she will allow to do anything for her as far as bathing dressing bathroom appointments etc. I am her aid and have been since she got sick. I got everything for her that she needed to be able to stay at home and not go to a facility. Any advice is veey much appreciated. I also wanna add that for 2 years prior to taking care of her i took care of another lady with copd and attended seminars and all appointments as well so i have alot of knowledge about the disease. Im just as scared as she is of the end stage and death. Please help.
I feel for you!
My Mom had a stroke 4 years ago, 9cms of her brain died. It was ischemic, so pack of oxygen. She has respiratory failure all of the time. She has 15% lung capacity and is currently in Isolation with pneumonia with cold extremities. We discussed that this Tuesday I am making all the decisions because she used to try and get out without being better. It only makes them worse.
Email me if you want to talk.
[email protected]
I am also on COPD Caregivers ONLY on Facebook
My heart breaks for you. I too have a messed up family. I know how much you hurt. I too have that family. My daughters don’t help me at all. Not even phone callI’.
Crying all nite.
Will be in touch tomorrow. I CARE!
LOve
I am in my last stage at 27/30% cant sleep gain alot of weight use the bathroom at lot I am scared not afraid to die just got depressed/nerves are shot my biggest fear that when I start not being able to breathe I will go nut s that scares me
Hang in there Pam. I’ve been down that road myself and with others. Hospice will make you comfortable and you will not suffer breathlessness. Your mind goes into a quiet sleep before you pass.
We never got Hospice because when you do hospice it means you no longer call hospital when you can’t breath. Instead hospice makes you comfortable but doesn’t give you medicine like antibiotics. So we never had hospice.
My husband died this week. His oxygen suddenly was reading 65 and that was with the ventilator on. So called 911 and was thinking it was the usually deal where he has pneumonia and he would be at hospital for a week and come home. However he also has fluid on the lungs. Suddenly he started having hard time breathing and blood pressure dropped very low. They gave him a lot of morphine so I believe he was feeling no pain. They said we should just take mask off and let him go because he was gone basically. My husband did not want the tube down the throat because doctor said once it goes down it wont be coming back off. So they took ventilator mask off and he died in a hour. It was very hard for my kids and I to watch. He wasn’t suffering I made sure he had a lot of morphine because that was my main concern.
In conclusion I would say I was glad there was no big suffering. I had heard stories of people being in hospital screaming HELP me for weeks and being blue. It was not like this at all. Also I want to say if you don’t have the Trilogy Ventilator get it. I know that kept my husband alive a extra year or so. It does all the work for the lungs.
Good luck everyone
I am so sorry for your loss. I don’t think we ever get over helping our loved ones through the final stages of this awful illness. I lost my mother in 2001. I had hospice for two weeks before she was gone. This allowed her to have loved ones at her side at all times.The last 48 hours were the worst as she could no longer talk and had what is called the death rattle.I laid in the hospital bed in our home with her and told her it was time to let go.Even though I was laying next to her with my arm around her, I was shocked when after asking my brother to stay with her for a few minutes so I could have a cup of coffee and after I left the room he got my husband and they came to the kitchen to tell me she was gone. 2 1/2 years ago I lost my brother to COPD, he thought it was pnemonia and called 911. He was hours away from me so I got my husbands meds (yes 4 COPD). They had entibated him before I got there, 7 days later I had to let go.It was hell for all. Now my husband is in end stage COPD and I am keeping him home with the help of hospice.It won’t change the outcome but I can give him medication to keep him comfortable when needed, not when the clock says it’s OK, and when needed 24hrs a day,I can get a RN to come, a very welcome change over the last 16 years.I indeed feel every care givers pain when no matter what they do their loved one won’t eat, the fight with bed sores and just the real need to let their loved one know he or she isn’t a drain on them though you are hiding your fears,tears and exhaustion. I have to know that when the end comes he will at last be out of pain,this isn’t the first husband I have lost. 34 years ago my then husband died of cancer. I will be here for my husband as I have tried to be there for many loved ones as they passed. There are no rules for this, we just do as you did, love and care for them the best way we know how. You as anyone who is going through what you have will have my prayers and deep respect.
My dad is 72 and in the end stages of copd. Like many, he’s a denier. He’s smoked since his early 20s and never thought it would catch up. He still denies this has anything to do with smoking. He tells us he’s getting better. Last year, after much weight loss and breathing issues he was diagnosed with MAC and COPD. My husband of two years and I moved Dad in with us. Today his primary doc recommended hospice. Dad still smokes. He is pretty much down to eating only ice cream and drinking Ensure clear. This man was the most wonderful father anyone could ever ask for. I only hope and pray we can make these last times easier on him. In the meantime, I would be lying if I said this wasn’t putting stress on my job and marriage.
My brother was given 48 hours to live 2 days ago they have put him on steroids and he is now eating and drink g. Such a change.
Hey everyone my I’m caring for my dad that has severe copd severe emphysema cor pulmonale hypoxemia polycythemia he was just discharged from the hospital 3days ago with these diagnosis. He is so on 24/7 oxygen now at 2L he has 3 different inhalers and also a nebulizer 4 times a day he also has hit blood pressure medication now. What can I expect as far as life expectancy for him. My dad is strong minded so he still able to move around through out the house.
I am going through end of life COPD with my Mom now. I came to this page hoping to find some clues to how long she has. I know in my mind that it is unpredictable, but her personality has changed over the last couple of weeks and I just hate the not knowing.
She is in Hospice in an assisted living facility, but is unable to stand without being so out of breath that it would be like a normal person running up a mountain.
I just wanted to know some signs to look for. She is scared to death of the thought of not being able to go to the hospital, but I feel like many of you in that I would want to be around loved ones instead of the hospital where the atmosphere is just clinical. There is nothing that can be done but keep her comfortable when the time comes and hospice will do that.
Hi everyone, I have 34% lung, and find what bothers me the most is thinking that I’ll take my oxy and try to repair something around the house, but I cant because I get to weak in the arm’s and legs.
and then I get mad at myself..
I cant get it in my head that I have a problem. I must be slow to learn.
Doug
Oh, Doug. I have CFS/ME and I continually plan to do more than my illness will let me do. I think it’s just a part of being sick and having been healthy. Your wish to do more – your desire to help by fixing things in the house is pure Love. I hope that this idea makes you feel better even if it can’t make you more able. I have been sick for 20 years and know well what you are going through. — Brenda
Hello my mum went into hospital Thursday 23rd with bad breathing due to her cops. She deteriorated and we were told the next few days are critical and she probably won’t be leaving. My heart broke as I lost my dad last year to dementia with lewy bodies.. my mum has had it since 1994. But Sunday she seemed to have got some life back into her. She’s on oxy and nebulizer. They also found nemoneia in her lungs. I was just wondering with all your experiences what do you think her chances are? Sorry to hear and read all your experiences God bless you All x
You just never know. I have COPD and am on oxygen 24/7 and have had pneumonia and respiratory failure three times in the past 3 years and twice they said I was dying. Last time it even went septic on me. I just keep plugging away but here I am this week with another infection and wheezing and coughing my head off. On azithromyacin and prednisone and nebulizer for 3 days but its not getting better. Will probably end up in the hospital again. I think a lot has to do with state of mind and how attentive your healthcare team is. Im very fortunate that my healthcare team is very good. I wish you luck and remember to take care of yourself too!!
My mom is there. She is 69 years old and for the last 3 years I have moved back home (I am a single 40 year old guy) to take care of her. Up until 6 months ago, she could still get up on her own, make coffee, use the bathroom, shower on her own. Sadly these past 6 months that has all changed. Every morning before work, I make sure O2 machine is on, back up machines are charged, has 2 cups of coffee, her meds, and water for the day. My nephew brings her breakfast every morning before work, and then when I get home from work at 7pm i make dinner and begin the process again. getting night meds, getting water, taking her to the bathroom, just trying to keep her calm and anxiety free. The past month, she has started to become afraid to sleep at night. I sleep on a couch in the living room 15 feet from her. When I hear her gasp for air in the middle of the night i am up. If I hear her cough I am up. She can no longer make a meal or cup of coffee on her own. She is on oxygen 3l 24/7. She takes prednisone, xanax, and small doses of morphine to help with the breathing. Going to the bathroom is a nightmare. She gets so winded and anxious it kills me. It kills me when she says she’s afraid to go to sleep. I am not sure if its because she is afraid she won’t wake up? Or if its the fact every morning is a struggle. I don’t want to use a nursing home as I hear horror stories of how loved ones are treated. I know she is scared as am I. I have 3 siblings, all of which are married with kids. I am single and kidless so this has fallen on me. My 1 day off is spent at Dr. Appts and I literally have to plan a day away months and months in advance to get someone to cover me. But given her inability to even use the bathroom alone is worrisome. She makes statements under her breath that I can’t make out or don’t make sense to me. I just don’t know how much longer I have with my rock and soul and to be honest, I may be more scared than she is.
We are going through a similar experience with my dad. My mom is there to take care of him but she is unable to lift him so a team of us have to assist. We just put him on Hospice on Monday which has offered some help. Hang in there Shawn! You are doing a very hard thing but sounds like you are doing it well. She appreciates this more than you know!
Oh Shawn, my mother is in a similar situation. My sister and I got a caregiver, at first just three days a week, three hours a day. Then our mother broke her hip and can’t walk so we have help every day. Now it’s very bad and it’ll be 24/7. She’s going into hospice and there’s on-call help 24/7 – this is in Rhode Island. That is very helpful. We promised that we’d not send her to a nursing home. Home hospice is much better, much kinder. But not all Hospice Agencies are excellent.
Hi, I was reading your post and I can totally relate to this. My dad is in the same position, he is unable to get out of bed himself and needs help with everything. He does not eat, only drinks. It is very worrying as it was a sudden decline in the past 8 weeks, unable to walk or do anything and is anxious. It is hard to know if things will get any better 🙁
You’re doing a good thing, Shawn. Many parents end up dying a alone. I have watched with my own eyes and hope I will have someone at my side when that day comes. Keep going for your MOM!
May I point out that the dying patient is still a living individual?
Hospitals are UGLY in their appearance and IMPERSONAL. When a friend’s relative was dying, I took into the hospital a CD player and a CD of favorite music. She enjoyed this for some days before the end, when she requested silence.
When my relative was very ill, I took in a colorful quilt that I spread over her bed while I visited – she loved the vivid colors.
It is great that comforting the body is stressed in this article — may I offer the idea of comforting the personhood of the individual in the bed, who misses her home and elements of her life even while dying?
Baby brother 47, with COPD,had heart attack and literally dropped dead. He showed signs only about 9 months before he died.Many hospitalizations and ICU visits…
I’m so sorry for all of you. My heart goes out to you, and give you credit as well. Not everyone can do what we are or have been. I am my 90 year old moms caregiver, she has COPD…. and now dementia, it’s getting harder and harder everyday. Seeing her mind and body deteriorating at the rate it is now is truly heartbreaking. She’s been with me and my husband going on 8 years. Most of it very pleasant enjoying her being with us. She had a desktop computer, a tablet for games she enjoyed. She forgets how to turn them on. She has a small refrigerator, she still goes in for some fresh fruit, or applesauce, juice etc. There’s even a water cooler for fresh water.
Now she’s like my little girl, the look of total trust in her eyes. Each day is very precious and I’m trying so hard to do what’s right for her. I work full time, I see her before I leave, place a something for her to eat, her meds and water next to her, call her from work….. she assures me she’s taking them as she should (most of the time now, no, including her inhalers) she’s determined not to go to the hospital. Luckily there’s no pain at all, just sooo very tired. I check on her
She sure loves her TV shows…….
Bottom line….. We love her, she’s happy, pain free and home. I will keep her safe and comfortable, or make other arrangements at our home for whatever is needed.
Thank you…. for your site.
Bless you for caring so beautifully for your mom. I’m dong the same and it is so heartbreaking.
My mom is 69 and has been on oxygen for over 6 years. She has been on 5 liters for almost a year and a half. Her lungs were at 42% and now she is around 28%. She only gets out of bed to use the bathroom. She hasn’t left her house in almost 4 months. She goes through 4-5 ventolin inhalers a month. She won’t quit smoking. She refuses to go to the doctor. I don’t know what to do anymore as I am her only caregiver, I have been doing this for 18 months. Can anyone give me any advise?
My mom past away 19th Feb. I looked after her for 12 years.she smoked till the day she died. It was very quick to be fair, respiratory failure. My advise is get as much help as you can. My poor mom ended up wearing nappies and towards the end hardly ate. She was just so out of breadth. I’m lost without her, although I looked after her the following days after her passing, I realised how much I still needed her. Just for being there. Good luck sweetheart.
Have a doctor sign her up for hospice, or call hospice and have then come evaluate her. They will help you. And it is all paid for by medicare.
I feel your pain Teri, you MUST take care of yourself as well. My Mom says she has stopped smoking but she will sneaks and smoke, all the while we as their children suffer in silence having to take care of them, as they have self inflicted themselves with nicitine. It makes you bitter, but still you don’t want to see them suffer in their last days. Prayers to you.
My mom is in her fourth stage several years now. Her feet have been swelling. ???
my ex-husband spent the past 3 days in a delirium. Was like taking care of a 2 year old. He seems fine today but a bit paranoid.
Hi my dad is 75 he has COPD. He has started to eat less and sleep more during the day. He has bad memory can’t remember some immediate family. He forgets to take his meds. And sometimes forgets that he has took it and take it again. As a caregiver what should expect next. Thanks Brandy
My husband has COPD and it hard to deal with. I didn’t want him to suffer. He has been getting worse I see the change in him. He can’t take a shower without having a hard time breathing. He can’t walk from on end of out apt to the other end our app isn’t not even 600 feet. And within the last month he sleep he stay’s in bed he doesn’t get up. Maybe to get something to drink his eating habits have changed.He’s in and out of the hospital about every 2 week’s now.and the last time he came inches of passing away on me. I’m so scared. And I think he knows. It has took me a long time to just to be able to read about COPD and the stages. I can’t bring myself to read the stage. I have been with my husband for a very long time. We were high school sweethear’s and we both our 55 now. I just can’t even begin to know what to do. Can someone please tell me the truth about stage 4 I need to know. God I know he can’t be leaving me k. It just can’t be.
My father is 68 years old. He has end stage COPD and admitted in MICU since 11 days. He didn’t show any sign even on the day before his admission in hospital. He went to his office and was completely normal. He was admitted for LVF and COPD and now the other organs have already started malfunctioning. He has stopped urinating. Dialysis is also not helping in this condition. The doctors have told us not to keep any hope but they’re still trying.
His health is deteriorating day by day. I’m too young to lose him. I wish he had told me about his problems before since he knew it but never told me about this. I’m praying for some miracle because I have no one other than him. He’s the closest person in my life. I hope he recovers soon.
I would like some advice as what to expect and more or less how long this would last.
My dad will be 76 years old soon, He has been suffering from COPD for about 9 years now.He was admitted in hospital with a lung infection he also only has 28% lung function and heart failure . the doctor has informed me that my dad has about 6 months life expectancy.Do I consider hospice ? Can he be admitted against his will ? what can I expect in the next 6 months ?
I live South of England and My Dad, who lives North of England, was diagnosed with lung cancer November 2017. We visited hime then just before he had gone through chemo. After his next check up he was told no further treatment could be given because of COPD on the other lung as well as cancer of the oesohagus . Since April My Dad had gone into hospital a couple of times for infections and breathing flare-ups. He was being cared for by his Sister, luckily. He asked if I could buy a train ticket for him to come and visit us, this was very unlike him, but he kept on and on…After I had booked his ticket his Sister had said she didnt think he was well enough as he kept getting out of breath. So with that My Husband and I (with kids)drove up to see him. I was shocked at his appearance. He had lost a tremendous lot of weight, He couldn’t eat, nor drink, and couldnt sit up, as this was more painful than laying down, He could only walk, well shuffle, 20 steps maximum before a breathing episode. Since my learning of this I have done much research, and like many of the other posts, he has gone through all of the ‘end of life’ stages list. A hospice was mentioned to him by a Dr which was called, he declined, but the Dr had said just go in whilst they fix his infection and make him comfortable, ‘some rest bite’, I call him every two days but this is beginning to be hard for me as he is started to get very confused and as well as this he is not being able to speak because of breathlessness. He has now been in hospice for 3 weeks. I called my Dad today and his Sister answered to say she had a call to say he another breathing episode and had another infection and was moved into a side room early this morning. This does not sound good at all. My Dads Birthday is in 6 days time and was going up then…My Aunt said she will call later with any update. I know My Aunt doesn’t want me to drop everything and us keep rushing up there…but Like everyone else, I’m surcharging for clues as to when. I have read all of the posts and thank everyone for sharing and my heart goes out to everyone this has effected as well as their loved ones <3 <3
Hi juju I am too searching for answers and send my love. I recently posted about my mum. This is truly awful when nobody can give you the answers you seek and we just have to keep guessing and waiting.
I just want to say, god bless us all, I to have COPD, I don’t know what stage I’m in Dr hasn’t told me, i am 85 years old, of doing so good,but I’ll hang in, God Bless.
My heart goes out to anybody caring for anyone with copd. This illness truly is a heart breaking mind messing abomination. My mum is 65 and was diagnosed around 6 years ago. She quit smoking straight away and for a while managed to get on with life a little she started with oxy therapy overnight and this would see her through the day. I could take her shopping help her garden ect. Then she started literally growing her own lung infections ecoli for one. She also suffered a lot with edema. Gradually she went from my strong mum to a very scared frail lady on oxy 24/7 numerous admissions to hospital some giving her only days. She would recover but always be worse after. I was her only carer and work were great letting me reduce my hours. But I still had to work and this was the hardest part having to leave her and not know how she was. She is also a co2 retainer so what seems like a little confusion can mean a lot more to me as I recognise the symptoms. In November last year she was admitted once again with high co2 and respiratory failure. She actually managed to pull through as she’s always said she doesn’t want to die because she doesn’t want to leave me. She decided enough was enough and we couldn’t cope on our own anymore and was fast tracked into a nursing home with 3 months to live. She has since been back into hospital 4 or 5 times and each time got worse. The nursing home are great in which they will sit her when she’s panicking and of course it means I can work. But I have a huge feeling of guilt that it’s not me there. I see her everyday without fail and every morning she texts me. Until last Thursday when I didn’t get the morning text. I phone the home 3 times and they told me she was asleep. I know that there’s something wrong so I leave work . O get there and she’s in and out of conciencness with oxy levels dropping to 56. She had given a sputum sample a few day before and Thursday the doctor sent antibiotics. Now normally I would have been on the phone to an ambulance but the last 2 weeks since bring discharged she had been in incredible pain in her lungs kidneys everyday she would scream out help me throughout the day and night saying she couldn’t go on anymore . I had a conversation with her while she was in her right kind and she told me that she’s had enough and doesn’t want anymore ambulances. She wants to go. So Thursday I layed with her holding her had and singing to her she would hum back they managed to get 3 antibiotics down her by emptying the powder in water and squirting down her throat. Friday morning she started to wake a little but was so scared and no idea about the previous day. He oxy started to rise a little but she was extremely hypoxic and probably co2 through the roof. She is currently drifting in and out conscientious hallucinating and talking rubbish. I have no idea what’s happening but I love her so much and when she’s like this I don’t think she’s in any pain. I don’t know the outcome I just know I will be there with her.
Hi there
My mom is 69 and exactly the same as your mom. It’s like you talking about our life.
It’s scary – a part of me would like my mom to slup away peacefully so she has no more pain… frustrating. Big hugs to you. No one knows …until they in your shoes. It’s heartbreaking
To tdv thank you i know its hard but stay strong x
Hi. My mom is at the end stage also. She is hallucinating, stopped all nutrition and is in denial what is happening to her. She has been having nightmares and is scared of dying. She believes she can get better and just come home. It’s heart wrenching for our family to watch and we are being as supportive as possible. My heart goes out to you and your family as I know to well of what you are experiencing. God Bless. Terri
Terri, sending my love to you and your family x
I feel the pain with you . Hurts so much and I’m dealing with this illness with my love of my life right now.
My Mom is 72 years old. Started smoking when she was 13 at one point did 3-4 packs a day. Now she has COPD refuses oxygen and refuses to take her meds daily has not used her Asthma like unit for years. Is vicious and cruel to me and my family with her outbursts which she then “can’t remember “ will not go to the doctor and lives in denial there is anything wrong. She has violent hacking coughing fits all day and night. Has anyone ever heard of this or is living with it now? My family and I live with this every day and we are at the end of our sanity
Dear Brian, The out burst or anger or depression or quite normal with anyone with COPD and they do not remember them.Try not to take it personally it is usually out of fear or frustration because she has no control over what is happening to her because she knows she is dying and can really do nothing about. It sounds like it is time to call in Palliative Care for her and they can help you understand more and help you work though a lot of this.
My mom is 51 and has been stage 4 copd for about 3 years now. She stays with me and she’s refused to quit smoking and its tearing me apart literally watching her die a slow death. I just wish she’d try to quit and try to get a transplant to get her life back. I’m afraid she might be approaching the end. She’s been on water pills for years but she recently got a pretty bad cold ( No pneumonia or anything.. xrays were clear) and now all she does is cough and sleep. Constantly sleeping. She does have as appetite though. Do you all with experience in this feel it’s just the child tiring her out or do you think I need to prepare myself for the worst? This is the worst feeling ever. Especially since I didn’t see her as much as a child and now that she’s in my life consistently I feel like my mom is being taken away from me all over again. What so you all think?
Hi all. I need advise as we are all losing it. My dad is 71 and has severe COPD. I look after him. About a month ago he started bleeding bad. Sometimes just a little and then a lot. Sometimes only blood sometimes clots as well. We started with oxygen a week ago. Lots of other meds as well that he has been on for some time now. Atleast the meds help. But what is up with the bleeding? Is this now the end?
My mom is 82. She had a cerebral stroke a few years ago, which made the Alzheimer’s she already had kick in to a higher level. She’s been in a nursing home since her stroke, and has now developed copd. She used to smoke until about 15 years ago. Anyway, she got pneumonia about 6 weeks ago, and can’t seem to completely shake it. She’s on oxygen quite a bit now, she’s not using her walker to and from meals, she needs to be pushed in her wheelchair. Normally she’s up
Normally mom is up using her walker. Then she will get a cough and go back to needing her wheelchair. This has gone on now for a couple of years at this time of year. I haven’t been told what stage she might be I. Has anyone here had the same type of experience with their lives one? I’m trying to prepare myself the best that I can. My mom is my best friend, she raised 3 of us as a single mother and we are a close knit family. I don’t know what I’m going to do without her, but I want to be the best daughter that I can be in her final years. Does anyone know if a way to find out how long a person may have to live with this copd? Thx everyone. ✌
My Mom is in the hospital with shortness of breath. She is now on oxygen all the time, and her weight is down to 98 pounds. She can still walk around some, and she lives alone. I’m 5 hours away and just got home from visiting with her. She doesn’t want to move closer to her family, she likes where she lives even though she is alone. Be grateful you have a Mom that loves and cares for you and is your best friend. Not all Moms care for their children.
Hi my boyfriend who was at the final stage off copd.
His aunt woke yestarday morning and found him passed away on his room floor without his oxygen mask on .would he have suffered for long??
I was reading up on the final stages of COPD and saw so many comments from the families caring for these individuals. Many sharing their personal stories about their loved ones, watching them suffer with a disease that has no cure and progressively worsens until the time of their death. I’m 53 years old, I have three beautiful daughters and a step son, a loving wife of 30 years and a handicap brother I care for. As I read all the stories about those most effected by this illness, I didn’t see any from those actually suffering from it, I was researching the final stages of COPD because I wanted to know what to expect as I go into these last stages. The hospital visits are more frequent, the coughing sometimes just won’t stop and then the shortness of breath is like someone sitting on your chest, the fluid in your lungs builds up and makes you feel like your drowning, deep breaths does nothing to make it go away, simple things like walking a short distance or short stairs leave you completely out of breath. The worse part is none of what I just described and not even the knowing your dying part. It’s watching those that mean most to you, watching you die slowly every day., deteriating to a point that you are no longer the care provider but a burden to everyone. You see the hurt in them, the helplessness they feel, the regret , uncertainty and when they speak of pain… I see more in their eyes than that I’m exoeriencing. What you may ask can you do to help those that have this disease..? There is only one thing you can do… love us for as long as we have left.. and remember the good times. Praise be to our father that’s in heaven and the mercy he has on our unrighteousness.
I am getting closer to the end of life myself and I can only say that I have discussed this with my wife and kids & when it is time that I want to go with dignity and not suffer. We have things in place and it isn’t wrong to think this way.
You’re not a burden. My father passed away two months ago and I wish I would have had a chance to tell him that he was never a burden to me and that I loved him.
My mom has COPD I AM 35 my moms 65 and it’s just not fair …. I care for her and I’m a single mom of 4 I love her so much these last stages and seeing her suffer kills me inside this Sickness is unkind seeing a person you love struggle to just breath haunts me my moms been on life support a handful of times doctors say she won t make it and Yano what she does I feel she fights for me and the kids I feel terrible for her
My father just passed away with severe COPD. Truly a cruel disease, and my heart goes out to any family member or persons suffering with this.
My dad was on a ventilator for 7 days and then he had a tracheostomy because doctors told us it would be more comfortable then being intubated. And he was! Problem was after his successful surgery he was moved to an acute rehab hospital where under heavy medication he passed away within 3 days. I need to know how those opioids affected him during the time of death. He was on Ativan and Morphine. I wonder if he stopped breathing or did he struggle, I just don’t know because he was on the ventilator which technically would’ve been giving him breaths and oxygen regardless. Anyone with similar situations? Looking for any clues or answers. Thank you.
Hi Mel, My Dad passed away on April 11. What a horrible way to go. In the end he was yelling “help me, help me” because he couldn’t breath. I would love to talk to you about this.
Hi Mel, I have also experienced a similar situation. Would like to talk to you.
I just found out that i have copd i dont know what to do or what stage im at. I quit smoking right away but im afraid and i dont like doctors.what should i do?
Anxiety is a huge struggle for those dealing with COPD, especially in more advanced stages. This blog had a lot of helpful information for me. Hope it helps! Thanks.
https://blog.lptmedical.com/copd-and-anxiety-how-to-find-peace-of-mind
Hi folks. I’m sorry to hear of your experiences! I am 64, been told I am at end stages of COPD. Doctors say I don’t have long. I’m not sure who to believe and trying to get advice as to my life expectancy. Doctors say weeks. I am ashamed to say I’ve smoked for 50+ years but proud to say none of my 3 adult sons smoke. Any info you can share with what little you know would be great. First diagnosed 10 years ago and my doctor said yesterday end of life <2 weeks. Thanks. EM [email protected]
have copd and having lots more problem breathing is there any thing in the end they can give you to make it faster and let painful
Hi I don’t know where to begin.I just buried my father 3 months ago he had throat cancer.He was doing really well after all the surgeries until he found out my brother who is 46 was in ICU because of COPD.My father was stressing and 2 days after my brothers stay my dad was found on his bedroom floor.My brother came out of it and just in time to be at the funeral.I delayed it hoping he’d be released.Well my brother has only 18 percent of lungs.He’s at my home now and is on a list for transplant.Every night I wake up to his machine on or the sounds he makes to gasp for air or to him coughing.Im worried he’s not going to make it.Im 43 and single parent of 6 kids and I stress everyday because I have no one to share my worries to.I am trying to stay strong for everyone and live everyday now trying to make it normal fighting back tears.I know he’s suffering but he says he’s fine and feels better.Oh also he never went to the hospital because he had no insurance.That was his first visit that he was told 18percent.He smoked for 2 yrs onlyHow much time do y’all think he has?In 2009 I woke up to him breathing weird and making noises like he couldn’t breathe.I begged him to go to the hospital but he refused and said it would pass.It never did.Its been 10 yrs.
My mom has severe COPD and emphysmea. SHe is almost 80. Lately she has been very mean and saying things that she would not say, normally. Is this all part of the end stages? She is on oxygen 24/7 plus 2 inhalers twice a day. I do not know what to do with her being angry and mean. Just started getting bad within the last week. She lives with me and my family, she uses a walker, does not go outside of the home. She can not walk without the walker and even with it she is extremely out of breath. What do I do about the mood swings?
Is it painful, well when my COPD exacerbates it’s not so much pain on your mind as it feels like someone put an invisible plastic bag over your head. Now I’ve been around the block in life, I’ve been stabbed, shot, my kidneys shit down due to bodily traume after the stabbing and I will say this my first exacerbation episode I went through was the scariest thing I’ve ever experienced. I’d rather repeat anything I’ve ever been through than have to go through a flare up with my COPD. I sincerely hope anyone who knows a person with COPD or has COPD the best of luck. As soon as you notice the start of a flare up get to the hospital do not wait to see if it passes, go ahead and just go to the ER trust me it is so much easier and way less scary if you just go and get treatment before you get to the full blown gasping for air phase. If your feeling confused, light headed, or your breathing isn’t your normal just go and get treatment before you get to that bad. If you don’t have COPD and you have a friend or loved one with it if you want to get an idea of what they have or will eventually experience just put any old plastic shopping bag over your head and loosely snug it that would be what they experience.
Thanks for the information, very helpful for people like myself…. Doing the best I can to care for an elderly uncle with (end stage) copd and right side heart failure etc etc
It is a terrible disease and a very disturbing experience to have to watch, I can only imagine how hard it is on my uncle when he is struggling to breathe and meds are not giving the relief that previously occurred
Cheers!
Has anybody ever heard of administering a TAVi to relief the symptoms
Sat here with my mum in final stages of COPD next to me getting comfort from knowing that at least there are other people out there who know the gut wrenching pain this causes to the COPD sufferer and us, their carers/children.
Mum was told in July 2019 that she may not see Christmas 2019. She had exacerbations but always seemed to bounce back. In December 2019 she went on a syringe driver of OxyCodone and Midazolam and after 6 weeks came off it back onto Oxycodone tablets, with Prednisoline, Carbocisteine and Lorazepam and Ivabradine. Everything was ok until 3 weeks ago when she stopped being mum and was in pain. The syringe driver has gone back in but tomorrow they are stopping dexomethasone (steroid) as in the rare moments she is awake she keeps asking to be let go.
I have never felt physical pain through loving someone so much and watching them suffer as I am with mum. I am lucky to be self employed and been at her side from diagnosis through to now. I don’t know how others who have to work full time are doing it.
After being told we have a few days, three weeks later mum is still hanging on in limbo.
I never thought I would be in the place where I want my mum to pass but her suffering is too much. She is at home and we have regular visits throughout the day from carers, hospice, nurses.
Stay strong everyone. This page if nothing else has been an enormous source of comfort. No one understands this disease until they’ve been through it at a loved ones side. Mum is 67.
Hi, my husband has copd and congestive heart failure it takes everything he has just to was to bv the kitchen we have a one bedroom apartment so from the couch to the kit CD hen is maybe 10 steps and he has to stop. He sleeps alot do you think hes in the last stage has been in the hospital about 10 times or more this year. He just got out a few days ago from being in there 21 days. I have to help in the shower with him because it takes everything out of him. Just standing up is hard for him.