A geological comparison between Texas and Florida provided feedback on the effects of respiratory care protocol implementation
A group of Orlando, Fla, area networked hospitals began their effort to implement respiratory care protocols in 1988 with execution of protocols applicable to patient assessment and oxygen therapy. In late 1996, a more focused project was initiated to implement additional protocols for medicated aerosol therapy, bronchodilator therapy, and bronchial hygiene therapy in the networked hospitals in an effort to reduce misallocation of services.
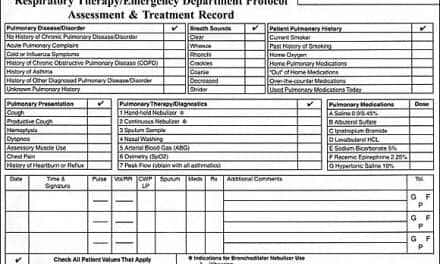
Over a 12-month period, regular in-service education programs were conducted for the entire respiratory care staff in preparation for progressive protocol implementation. The primary focus was on communication skills, assessment skills, and indications for each modality for which a protocol was planned. During this time, emphasis was also placed on gaining a consensus on aerosol therapy among physicians, nursing practitioners, and RCPs based on the American Association for Respiratory Care (AARC) Clinical Practice Guidelines. Supervisors and educators were given additional training to prepare them as facilitators and to provide insight as to the rationale for protocols. A three-phase pilot program was initiated to implement approved protocols. In Phase I, following a formal assessment of each patient, it was possible for designated RCP assessors to make some changes in therapy (ie, switching qualified patients from small volume nebulizers to metered dose inhalers [MDIs] with spacers). Other recommendations for changes in therapy were communicated via a conspicuous sticker placed in the physician orders section of the patient’s chart. In Phase II (September 1997), the number of assessors was expanded to include the supervisory staff. They began communicating with physicians in the progress notes. Utilizing the Problem Intervention Evaluation Recommendation (PIER) format, they informed the physician of automatic changes that had been made in therapy and communicated additional recommendations for nonautomatic changes in therapy. In Phase III (February 1998), all staff RCPs began making automatic changes in regard to modality, frequency, renewal, and discontinuance of therapy once the physician had written the initial order. The chart sticker was eliminated and changes were communicated only in the progress notes. This daily “customizing” of the treatment plan was done using objective and approved criteria.
Between Phase II and III, participating RCPs were asked to complete a survey that had previously been utilized in an Austin, Tex, protocol project.1 Although the survey had been previously used to measure RCPs’ perceived educational needs, opinions, and attitudes prior to the initiation of an education program and protocol implementation, it was anticipated that the survey could provide valuable mid-project feedback. Of additional interest was a comparison of the results from the Texas project with the results from the Florida project.
Methods and Materials Materials
The published survey,1 which was not modified, was undertaken with the following objectives: to identify the knowledge level and the extent of clinical experience with protocols among the targeted RCP population; to identify, from the RCP’s point of view, the extent of additional retraining necessary; and to identify RCP opinions and attitudes on learning methods, barriers to implementation, and the effects of protocol implementation.
The results were intended to guide the ongoing training program and to identify possible barriers to successful implementation of Phase III of the program. Geographical variation in practitioner perception was of additional interest. It was anticipated that this collaboration would lead to a sharing of ideas on how to address variation in practitioner expertise, overcome barriers, and maintain momentum in projects that span several years.
The survey was distributed to each RCP employed in the four participating hospitals in the Orlando area. The surveys were completed anonymously with RCPs indicating only their principal employer. Completed surveys were forwarded to the survey’s original author for analysis.
Statistical analysis was performed using SPSS (SPSS Inc, Chicago) for aggregate frequency distribution and descriptive statistics (mean, median, mode, minimum, maximum, and standard deviation). Frequency distribution by hospital was analyzed for some questions.
Results
The Florida RCPs’ rating of their knowledge of respiratory care protocols is shown in Figure 1, with a mean (SD) of 3.173(0.667). Figure 2 shows how the Florida RCPs rated their clinical experience with protocols, with a mean of 3.284(0.711).
 |
 |
| 1 = No Knowledge 2 = Minimal Knowledge 3 = Fair Amount of knowledge 4 = A Lot of Knowledge |
1 = No Clinical Experience 2 = Minimal Experience 3 = Experience with 1-2 Protocols 4 = Experience with >6 Protocols |
| Figure 1. RCP knowledge of RC protocols (T/n=75, F/n=81). | Figure 2. RCP clinical experience with RC protocols (T/n=75, F/n=81). |
Overall, 26.5% of the Florida RCPs indicated a concern that review and retraining would be inadequate.
The respondents chose a preferred learning method only when one choice among five could be selected. Overall, lecture with questions and answers had the highest preference among the Florida RCPs and independent study was selected with the lowest frequency. The five learning methods also were ranked as alternate choices by the Florida respondents. Skill workshop with practice sessions was the highest ranked alternate.
Figure 3 shows what the Florida RCPs believed would be the biggest barrier to implementation of protocols in their respective hospitals. Overall, physician acceptance was ranked as the number one anticipated barrier.
|
|
1 = Physician Acceptance 2 = Nursing Acceptance 3 = RCP Acceptance 4 = Administrative Acceptance 5 = RCP Review and Retraining 6 = Heavy Use of PRN/Pool RCPs 7 = Inadequate RC Staff 8 = Other |
| Figure 3. Most significant barrier to protocol implementation (T/n=75, F/n=79). | |
Of the 83 responding Florida RCPs, 92.8% supported the concept of respiratory care protocols.
Discussion
Based on the fact that the Orlando area project was already in Phase II at the time of the survey, it was anticipated that RCPs would rate their knowledge and experience level higher than their Austin peers. Among the Florida RCPs, 87.7% responded that they had at least a fair amount of knowledge on the subject of respiratory care protocols. This compared to 59.2% of the Texas RCPs. It follows that the Florida RCPs were considerably more experienced in clinical application of protocols. Only 9.5% responded that they had minimal or no clinical experience with protocols. This compared to 61.3% of the Texas RCPs. Of the responding Florida RCPs, 40.7% indicated that they had clinical experience with more than six protocols. Since the Orlando area network had four protocols implemented at the time, it was encouraging that such a large percentage of the RCPs had previous experience. Despite the considerable knowledge and experience level of the Florida RCPs as compared with the Texas RCPs, looking at each individual hospital did highlight some additional educational needs as well as opinions that warranted follow-up meetings with the staff.
The perceived educational needs of the Florida RCPs were less in each of the 11 subject areas compared to those of the Texas RCPs. Since the Florida RCPs had considerably more experience with protocols, they should have been more aware of the skills needed. Interesting, however, was the fact that the Florida RCPs rated their highest educational needs in the same areas that the Texas RCPs rated their highest needs. The greatest perceived needs were in radiographic interpretation, pulmonary function testing (PFT) analysis, and electrocardiography (ECG) interpretation. While Florida RCPs consistently perceived their need to be less in each of these three areas, the related need was considerably higher than in any of the other eight areas.
There are several possible explanations for this outcome. First, radiography, PFT, and ECG may not be skills that are called on frequently in the delivery of routine respiratory care procedures. This may explain why the RCPs believed that their prior education warranted significant reinforcement. Second, even though radiography, PFT, and ECG have been deemed critical to the implementation of protocols per the Model Curriculum for Assessment Skills,2 educators may not perceive them as important as the other eight topic areas. In the Austin area project, only bedside PFT was included in the initial education program. In the Florida project, radiography, PFT, and ECG were not included in the initial education program. Retraining on radiographic interpretation and PFT is currently being planned. ECG monitoring is not routine on patients outside of the intensive care units and ECG results do not tie directly to any of the protocols. As a result, retraining on ECG analysis is not planned at this time.
Overall, 26.5% of the Florida RCPs indicated that review and retraining would be inadequate. Even though this was considerably less than the Texas RCPs (45.3%), this percentage may seem high considering that training had been ongoing for more than a year and the implementation process was proceeding successfully at the time of the survey. This may reflect RCPs who were newly hired and did not participate in the preceding education program. Even taking this into consideration, the results underscore the point that education is an ongoing process in any protocol project and must not have an end point.
The Florida RCPs had a stronger preference for lecture/question and answer as a learning method than did the Texas RCPs who had the strongest preference for skill workshops with practice sessions. On the whole, the Florida RCPs had nearly an equal preference for lecture/question and answer, skill workshop with practice sessions, and clinical practicum with a preceptor. As with the Texas RCPs, the Florida RCPs had a low preference for independent study. It is reasonable to conclude that RCPs with extensive clinical experience, which is representative of the Florida population, are more confident in their skills. Therefore, the continuing education they need may easily be addressed in a lecture format where they can have their specific questions and answers addressed. However, RCPs with less experience, or new hires, may continue to require skill workshops and supervised patient assessment and care plan preparation with a preceptor. Within the Orlando area network, each new hire must complete the orientation education modules and achieve 90% on a post-test. The new hire is then supervised by a department educator on patient assessment and care plan preparation per the protocols. The Florida educators agree with the Texas preceptors that this individualized attention is a key element in the education program. Once the supervisor signs off on the new hire, they may begin work. Follow-up and performance improvement monitoring is conducted by the educators and supervisory staff. Many of the Orlando area network’s new hires are graduates of local programs. To streamline the orientation process, the network protocols have been added to the respective curriculums through the work of an advisory council represented by educators in two local associate of sciences program, one bachelor of science program, and educators from area hospitals. The network educators find that the graduates of these programs are well versed in the protocols and accomplish the orientation program with greater ease.
Physician acceptance has been reported in the literature as a potential barrier to protocol implementation.3-7 Like their Texas peers, the Florida RCPs also predicted this to be the biggest barrier to implementation. Despite the Phase II status of the Orlando area project, the RCPs actually selected physician acceptance at a higher rate than the Texas RCPs (57% vs 41.3%). In Phase II, the Florida RCPs were communicating with the physicians in the progress notes utilizing the PIER format. A few physicians objected to the length of the RCPs’ notations in the progress notes. After some counseling of RCPs, documentation is now very brief using the PIER format and physician objections to the length of notations have been diffused.
In two of the Texas hospitals, physician acceptance has continued to present problems. The assignment of full-time RCP physician liaisons that work with physicians one-on-one shows early promise, but progress has been slow. The implementation of protocols in the Texas hospitals was distinctly different from the process utilized in the Florida hospitals. In the Texas project, physicians must order therapy per protocol, thereby triggering an initial assessment by an RCP. Following the assessment, the RCP designs and implements a care plan and subsequent assessments are scheduled every 24 hours. In effect, this implementation has led to therapy by protocol being the exception rather than the rule. In Phase III of the Florida project, all orders for respiratory care are automatically implemented per protocol and every patient receives an initial assessment and routine follow-up. Therefore, therapy by protocol is the rule rather than the exception. This unique approach has resulted in a very successful protocol program with measurable benefits.
In the original survey, the Texas RCPs also identified inadequate respiratory care staff as a potential barrier of some significance (36% of respondents). In the early stages of implementation, only one of the Texas hospitals perceived staffing levels to be a barrier. One year later, however, this picture has changed. The central Texas region is experiencing a shortage of qualified RCPs. Increased workloads have resulted in the inability to follow up on protocol patients on a 24-hour basis. Missed assessments have in turn led to physician discontent with the programs. The Orlando area project also encountered problems associated with inadequate staffing. In Phase I, despite the fact that assessments were scheduled only on order and then every third day, about 50% of these were being missed. This was responded to in Phase I by doubling the number of assessors and authorizing overtime if necessary. In Phase II, the number of assessors was further expanded by adding supervisory staff. In Phase III, all staff RCPs perform their own assessments. When workloads are calculated, time is allotted for the number of assessments due during the shift. This effectively reduces the procedure load to allow time for assessments. Feedback from RCPs indicates that this approach has been satisfactory and, at the conclusion of second quarter 1998, the question and answer team reported that 86% of assessments had been completed during the quarter.
It was encouraging to see that RCPs actively involved in a protocol implementation project remain optimistic. The majority of the Florida RCPs are experiencing an increased level of responsibility, respect/recognition, job satisfaction, and job security. In contrast to the Texas RCPs, however, a greater percentage of Florida RCPs reported no change in respect/recognition and job satisfaction. It is possible that these results reflect the opinions of RCPs with short tenure who had not experienced the transition that occurred in September 1997. It may also be possible that the Texas RCPs, with their limited experience, may have been overly optimistic as to the positive impact of protocol implementation. Follow-up interviews with Texas RCPs have supported this possibility.
Similar to the Texas RCPs, the Florida population also anticipated a positive impact on the appropriateness and quality of therapy, and the productivity and cost-effectiveness of the respiratory care department. However, as above, a larger percentage of the Florida RCPs perceived no change in these areas, perhaps reflecting inadequate feedback to the staff of program outcomes. A concern that was clearly expressed by the Texas population was that utilization of respiratory care would decline sharply (50%). This translated into uneasiness regarding job security. In sharp contrast, only 18.4% of the Florida RCPs believed utilization would decrease. In the Orlando area network, the utilization of basic respiratory care procedures did in fact decline by 10.5% (26,172 procedures) when comparing first quarter 1997 data (prior to present-generation protocols) to first quarter 1998 data (after present-generation protocols). This has occurred despite a reduction in the length of stay by only 0.10 days for patients categorized in major diagnostic categories 4 and 5 (pulmonary and cardiac diseases) and is impressive considering patient days have increased by 9% in the same period. From the first quarter 1997 and the first quarter of 1998, the network reduced its full-time employees by 10. This was accomplished primarily through reduced utilization of agency therapists. The survey results highlighted the possibility that the Florida RCPs may not have fully understood the impact of protocol implementation on departmental and institutional goals. Since the implementation of Phase III, outcome data have been discussed at staff meetings. Institution administrators have been invited to provide information on how positive departmental outcome has translated to the meeting of overall network goals.
Despite the apparent optimism of the Florida group, a surprisingly high percentage perceived that protocols were paving the way for nursing to assume responsibility for respiratory care procedures. Their level of concern was similar to that of the Texas group. While there were no reengineering projects actively under way at any of the Orlando network hospitals during Phase II, the Florida RCPs were aware of initiatives aimed at future elimination or decentralization of yet to be identified services. Additionally, it was known that respiratory care had been challenged to reduce the fiscal budget by 10% and to investigate sharing some services with nursing in new patient care units where nursing FTEs were expected to increase while RCP FTEs were not. Also, some of the RCPs on staff had recently been displaced from another area hospital as a result of decentralization of the respiratory care department. While it is important for RCPs to be fully informed, such information may cause a general uneasiness among respiratory care professionals. Such concern may have been reflected in the survey results.
Conclusion
The survey, although originally designed to be utilized prior to protocol implementation, provided valuable feedback in Phase II of a three-phase process. RCPs in the Florida project perceived their educational needs to be less than those of the Texas RCPs; how-ever, their greatest needs were in the same areas. This information will be utilized in the ongoing education process. In general, the Florida population remained optimistic regarding the impact of protocols on their role in the hospital and on the respiratory care department. The survey did identify groups of RCPs who were less optimistic about job security. This highlighted a need to provide regular feedback to the staff on the positive impact of protocols on quality of care and improved outcome and the tie-in to the overall organizational goals. Sharing results from the same survey conducted in two geographically remote areas creates the opportunity for project facilitators to share ideas on how to address variation in practitioner expertise, overcome barriers, and maintain momentum in projects that span several years.
Cheryll K. Hagus, EMBA, RRT, is assistant professor of the Department of Respiratory Care at Southwest Texas State University, San Marcos:Richard A. Hicks, RRT, is staff development coordinator of Respiratory Care Services, James Webb, MBA, RRT, is administrative director of Respiratory Care Services: Thomas Berlin, MS, RRT, is director of Respiratory Care Services at East Orlando Campus and Extended Care Division; Don Bartlett, BSRT, RRT, is director of Respiratory Care Services at Altamonte/Apopka Campus; and Owen Bass, RRT, is an instructor of Respiratory Care Services; all at the Florida Hospital, Orlando.
References
1. Hagus CH. Practitioner perceptions of educational needs and effects of respiratory care protocol implementation: a citywide survey. Respir Care. 1997;42:858-867.
2. Des Jardins T. A model curriculum for the “assessment skills” essential for the successful implementation of “therapist-driven respiratory care protocols.” In: Burton GG, Tietsort JA. Therapist Driven Respiratory Care Protocols: A Practitioner’s Guide for Criteria-Based Respiratory Care. Los Angeles: Academy Medical System Inc; 1994:102-118.
3. Bunch D. Therapist-driven protocols: overcoming the obstacles. AARC Times. 1993;17:47.
4. Clifford CP. The respiratory care protocol: a physician’s perspective. AARC Times. 1991;15:61-62.
5. Shrake KL, Scaggs JE, England KR, Henkle JQ, Eagleton LF. A respiratory care assessment-treatment program: results of a retrospective study. Respir Care. 1996;41:703-711.
6. Stoller JK, Michnicki I. Medical house staff impressions regarding the impact of a respiratory care consult service. Respir Care. 1998;43:549-551.
7. Hess DR. Professionalism, respiratory care practice, and physician acceptance of a respiratory care consult service. Respir Care. 1998;43:546-547.