Respiratory therapists and nurses handle most of the day-by-day care of tracheostomy patients, and these healthcare professionals need to know how to provide the best care to achieve the best outcomes.
By Bill Pruitt, MBA, RRT, CPFT, FAARC
Patients who are receiving mechanical ventilation for an extended period will have the oral endotracheal tube (ETT) replaced with a tracheotomy tube. The time period for this procedure is usually at seven days, although some institutions will extend this to 10 days.1 Having a tracheostomy enables a decrease in the use of sedation and facilitates weaning from mechanical ventilation.1 Other patients who may have a tracheostomy include those with upper airway obstruction, those needing airway protection due to traumatic brain injury or neurologic disease, or those needing frequent effective pulmonary hygiene to clear secretions.1 A tracheostomy also facilitates oral hygiene, allows for better patient comfort, provides for a more secure airway, and decreases the risk of tracheal necrosis when compared to the ETT.2
Tracheostomy is one of the most common procedures performed on critically ill patients.2-3 This article will discuss tracheostomy devices, procedures, care of these patients.
Devices and Supplies
Tracheostomy tubes come in various sizes and configurations and are made of polyvinyl chloride, silicone, or polyurethane. Metal tracheostomy tubes (silver or stainless steel) are rare but may still be utilized. Tracheostomy tubes usually have a 15 mm connector to connect to a resuscitation bag or ventilator circuit, a flange that allows for securing the tube to the patient’s neck (using sutures, twill tape, or hook-and-loop fasteners), and the tube is curved or angled at 90 degrees to follow the tracheostomy tract. Tracheostomy tubes can have an inflatable cuff to form a seal in the airway for positive pressure ventilation or be cuffless.4
Some tracheostomy tubes are fenestrated (meaning they have an opening through the side wall of the tube that can be used for allowing speech) or nonfenestrated (no openings in the side wall). Typical tracheostomy tubes will have an outer cannula and an inner cannula – which may be disposable or may be reusable (requiring periodic cleaning). The cuff is usually filled with air and are low pressure, high volume cuffs to reduce the damage to the tracheal wall. (Cuffs may also be designed to fill with water or will be made of foam and will passively expand to form a seal).4 Some tracheostomy tubes are extra-long to extend farther down the trachea and are often used in patients who have had a damaged tracheal wall (often from an ETT or previous tracheostomy tube cuff that was overinflated). Tracheostomy tubes include an obturator, which is a solid piece that fits inside the tube’s cannula having a bulb at the end. This is used to close the tip of the tracheostomy tube and aid during insertion of the tube. Once the tube is in place the obturator is removed.5
Procedures
The tracheotomy tube is put in place either by an open surgical tracheostomy procedure or by a percutaneous dilation tracheostomy procedure. Both procedures require special training, and during both procedures the ETT is left in place until the tracheostomy had been completed. The open surgical procedure is most often performed in the operating room (OR) under general anesthesia. This involves dissection of the trachea followed by an incision made between the second and third tracheal rings to allow for insertion of the tracheostomy tube.4 The percutaneous dilation procedure can be done at the bedside or in the OR. The percutaneous tracheostomy is a quicker procedure, less expensive, and does not require scheduling an OR suite so may be more timely.
During the procedure one clinician performs a bronchoscopy to visualize the airway – observing the passage of the guidewire, dilators, and tracheostomy tube—while the other clinician inserts the guidewire, dilators, and places the tracheostomy tube through the skin into the trachea. Complications for these procedures includes bleeding (the percutaneous procedure has less risk 1,4), pneumothorax or pneumomediastinum due to a false tract or perforation, esophageal perforation, tracheal ring fracture, or loss of the airway.4
Tracheostomy Care
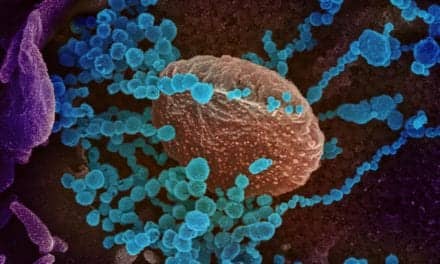
Manipulation of the flange, tracheostomy tube, inner cannula, and/or securing ties often causes the patient to cough (and sometimes expel secretions from the tracheostomy). COVID-19 precautions recognize that performance of a tracheotomy and care for a tracheostomy is an aerosol-generating procedure. In light of this, the person performing care of these patients should wear appropriate personal protective equipment including gown, gloves, face shield, and N95 masks or powered air‐purifying respirator (PAPR) systems.6
During the first seven days, the stoma (the opening for the tracheostomy) matures and begins healing. This period requires regular assessment of the stoma and frequent cleaning with dressing changes as needed.1 Keeping the peristomal area clean and dry is important to prevent skin breakdown.2 Since coughing is a frequent occurrence with tracheostomy care, suctioning the airway using the recommended guidelines for this procedure may be considered the first step. Closed-system suctioning is recommended to reduce possible exposure to air-borne pathogens like COVID-19.2
Cleaning the Stoma, Outer Cannula, and Flange
Tracheostomy care should be performed with sterile technique to prevent possible nosocomial infection. The stoma, outer cannula, and flange is cleaned with cotton swabs or a gauze pad moistened with sterile saline (0.9% NaCl). This is often done initially every 1 to 2 hours then as the site matures and heals, every eight hours at the minimum depending on the facility’s policy.7 The dressing placed around the stoma and under the flanges should be changed when soiled with secretions or blood and should never to cut as the cut edges of the gauze may fray or cause irritation.2
Cleaning the Inner Cannula
Tracheostomy tubes with a disposable inner cannula should have the inner cannula replaced. Nondisposable inner cannulas should be removed for cleaning then re-inserted. For cleaning, the inner cannula is removed and placed into a sterile soaking tray filled with either sterile saline or saline/hydrogen peroxide. A cleaning brush is used to clean the inner cannula inside and out. After cleaning, the inner cannula should be placed in a rinsing tray filled with sterile saline to remove any cleaning residue/fluid (hydrogen peroxide can be irritating to the skin).
The inside of the inner cannula can be dried with a sterile, dry pipe cleaner. After cleaning and drying, the inner cannula should be reinserted and checked to make sure it is secured.7 (Disposable inner cannulas have either a twist-and-lock feature or have clips that connect to either side of the outer cannula).
Cuff Pressure and Securing the Tracheostomy
Cuff pressure (with cuffed tracheostomy tubes) should be checked and maintained between 20 and 30 cmH2O.8 If cuff pressure is too low, positive pressure ventilation may be ineffective due to a leak and the risk for aspiration of secretions past the cuff will be greater. Too high of a cuff pressure may occlude the tracheal wall circulation and cause ischemia/infarction of the area. Twill tape or hook-and-loop fasteners is often used to secure the tracheostomy tube.
These devices pass through the eyelets on the flange and go around the back of the neck. They should be replaced when soiled. If two lengths of twill tape are used, they should be tied to the flange and the final connecting knot should be offset to one side or the other of the neck so the patient is not resting on this knot. (See reference 7 for more details.)
Changing the Tracheostomy Tube
Tracheostomy tubes are routinely changed as an infection prevention measure. Other times a tube may need to be changed to a different size/type of tube (ie, fenestrated or nonfenestrated, cuffed or uncuffed, larger or smaller size), if the cuff has been compromised on a cuffed tube, or if tracheal stenosis or tracheomalacia has developed.
The recommended timing for a change is 7 to 30 days after the initial insertion then 30 to 90 days thereafter.8 The first time a tube is changed the procedure carries higher risk since the tract is not mature, so a physician should do this. Once the tract has matured (usually after 4-6 weeks post-initial insertion), other professionals (ie, respiratory therapists or nurses) should be able to perform the change.8
Communication
A patient may be able to communicate verbally using a speaking valve (i.e. Passy-muir), tracheostomy button/cap, or finger occlusion. These approaches allow air to move around the tracheostomy tube and up through the larynx/vocal cords to enable the patient to speak. The devices have distinctive colors and should not be discarded to allow for periodic patient use and reuse.7-8 Speaking valves can be utilized with patients receiving mechanical ventilation.9-10 A speech-language pathologist is a valuable team member who can help with using these devices and with communication overall.2
Emergency Supplies
Accidental displacement of a tracheostomy may present an emergency situation. Recent and non-mature tracheostomy tracts tend to close quickly, making reinsertion of a tracheostomy tube difficult. Sometimes an ETT will be placed orally until the situation stabilizes and allows for continued ventilation/oxygenation.
A same-sized sterile, packaged tracheostomy and the next smaller size device should be available at bedside for replacement purposes. In addition, suction equipment, gloves, a bag-valve-mask and manual resuscitation bag, and spare tracheostomy tube ties/hook-and-loop fasteners should be at bedside. Some facilities also include appropriate size ETTs to be present in case a replacement tracheostomy tube cannot be successfully inserted.2
Special Considerations
Tracheostomy tubes bypass the upper airway and the normal heating, humidification, and filtering functions of the nose. Supplying warmed and humidified air helps in patient comfort but more importantly, aids in avoiding obstruction of the tube by thick, retained secretions. An obstructed tube is a critical emergency and risk reduction includes humidified air, removal of secretions by suctioning, frequent cleaning and maintenance of the inner cannula (if one is in place), and adequate patient hydration.8 Minor bleeding of the stoma is expected and should be manageable.
Major bleeding can occur if a tracheoarterial fistula occurs. This most often happens when the innominate artery is involved and can be due to the tip of the tracheostomy tube (or the tube cuff) rubbing and eroding the artery. This presents as massive bleeding and has a reported survival rate of only 14%. Repair can be done by a median sternotomy and ligation of the innominate artery.8
Decannulation (removing a tracheostomy tube) may occur in spontaneously breathing patients usually involves a gradual step down in tube sizes over days or weeks, or moving through progressively longer time with the tube capped—allowing the patient to breathe through the upper airway. Most stomas and tracheostomy tracts begin to close within hours of decannulation and are fully or almost fully closed within seven days.8
Conclusion
Tracheostomies are a frequent occurrence and patients with a tracheostomy take special care and attention. Although there are several possible problems/issues associated with a tracheostomy, with careful attention and appropriate action to reduce risks, tracheostomies are a safe and effective airway for those who need a “trach.” Respiratory therapists and nurses handle most of the day-by-day care and need to how to provide the best care to achieve the best outcomes for these patients.
RT
Bill Pruitt, MBA, RRT, CPFT, FAARC, is a writer, lecturer, and consultant. He has over 40 years of experience in respiratory care, and has over 20 years teaching at the University of South Alabama in Cardiorespiratory Care. Now retired from teaching, he continues to provide guest lectures and write. For more info, contact [email protected].
References
- Hashimoto DA, Axtell AL, Auchincloss HG. Percutaneous Tracheostomy. The New England Journal of Medicine. 2020 Oct 28.
- Parker, Parker LC. Tracheostomy care. Nursing 2020 Critical Care. 2014 Nov 1;9(6):38-41.
- Klotz R, et al. Percutaneous versus surgical strategy for tracheostomy: a systematic review and meta-analysis of perioperative and postoperative complications. Langenbeck’s Archives of Surgery. 2018 Mar;403(2):137-49. 4.
- Tracheostomy in adults. https://www.uptodate.com/contents/tracheostomy-in-adults-techniques-and-intraoperative-complications.
- From the OHSU website Trach Care Guide: https://www.ohsu.edu/sites/default/files/2019-03/OHSU-Trach-Care-Guide.pdf.
- David AP, et al. Tracheostomy guidelines developed at a large academic medical center during the COVID-19 pandemic. Head & Neck. 2020 Jun;42(6):1291-6.
- Tracheostomy Nursing Care. Wayne, G. Updated 2016. From https://nurseslabs.com/tracheostomy-nursing-management.
- From the UpToDate website: Tracheostomy Care. https://www.uptodate.com/contents/tracheostomy-postoperative-care-maintenance-and-complications-in- adults.
- O’Connor LR, et al. Physiological and clinical outcomes associated with use of one-way speaking valves on tracheostomised patients: A systematic review. Heart & Lung. 2019 Jul 1;48(4):356-64.
- Sutt AL, et al. Communication Success and Speaking Valve Use in Intensive Care Patients Receiving Mechanical Ventilation. American Journal of Critical Care. 2022 Sep 1;31(5):411-5.