A virtual reality (VR) simulation program at Cincinnati Children’s Hospital helped PICU staff hone their ability to recognize signs of respiratory distress and impending respiratory failure in pediatric patients, according to a study published in American Journal of Critical Care (AJCC).
Caring for patients at the bedside has long been the best way for nurses to develop clinical assessment skills. However, fewer opportunities for hands-on clinical exposure during training, orientation and onboarding, combined with increased reliance on technology and test results, have contributed to reduced bedside assessment skills early in nurses’ careers.
To counter these challenges, Cincinnati Children’s Hospital Medical Center developed a VR simulation to teach clinical assessment skills to newly graduated nurses, specifically focused on identifying pediatric respiratory distress and impending respiratory failure, including recognizing when to escalate care.
The study, “Impact of Virtual Reality Simulation on New Nurses’ Assessment of Pediatric Respiratory Distress,” details the curriculum design and outcomes compared with standard training.
Senior author Matthew W. Zackoff, MD, MEd, assistant professor of pediatrics, division of critical care, University of Cincinnati College of Medicine, is associate medical director of the pediatric intensive care unit (PICU) and co-lead for digital training in the Center of Simulation and Research at the medical center. He is co-director of the PICU Innovation Accelerator, which strives to design, implement and study innovative approaches to prevent and address critical illness.
“VR has a unique ability to create a safe environment for deliberate practice in the assessment of realistically portrayed clinical situations,” he said. “Our findings suggest the exposure to a VR curriculum may have accelerated transition-to-practice by enhancing new nurses’ abilities to recognize and interpret assessment findings.”
In the study, new nurses were randomly assigned to complete either an immersive VR curriculum or the standard orientation curriculum. A total of 168 nurses were enrolled in the study, with 83 in the VR intervention group. Most had worked in their unit for less than six months before the training session.
The VR environment, experienced through an Oculus Rift headset, replicated an inpatient hospital room with standard furniture, equipment and a vital sign monitor. The environment also included a virtual preceptor and a patient, both of whom were controlled by a trained simulation facilitator.
The VR curriculum consisted of three scenarios in which participants assessed the respiratory status of a virtual infant patient. The scenarios began with the same clinical prompt and then portrayed the spectrum of respiratory distress: no distress, respiratory distress and impending respiratory failure.
When evaluated three months and also six months after the training, nurses in the VR intervention group were significantly more likely to correctly recognize impending respiratory failure, identify respiratory distress without impending respiratory failure, and recognize altered mental status.
Source: American Association of Critical-Care Nurses (AACN)
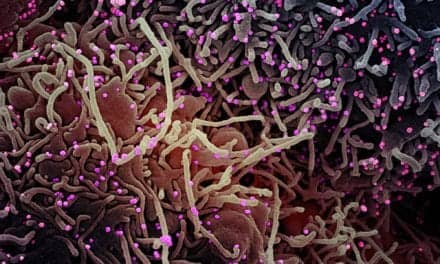
Image: Clinicians during a virtual reality session using Lumeto’s Involve XR software. Photo contributed by Lumeto, which manufactures a medical simulation training program. The Lumeto product was not used as part of this curriculum or study.