Each premature infant must be carefully evaluated before determining the proper use of anesthesia.
Premature birth is a crisis situation requiring emergency measures. A normal environment does not apply; neither do routine medical procedures. A very special care situation exists for the entire health care team. Infants classified as having low birthweight or as being premature are unique in that they present challenges that must be addressed when anesthesia is required for surgical procedures. Immaturity and disease compromise pulmonary dynamics. Statistically, there is a higher risk of cardiac arrest during surgical procedures requiring anesthesia in these infants than is seen in other infant and adult populations.1
Neonates born at 31 to 35 weeks’ gestation typically weigh 1 kg to 1.5 kg. Those born at a gestational age of 26 to 30 weeks usually weigh 600 g to 1 kg; at less than 26 weeks’ gestation, they may weigh only 400 g to 600 g. The smaller the infant, the more likely it is that incomplete pulmonary development and architecture will result in respiratory distress syndrome (RDS).
RDS often results in mechanical ventilation of the infant. Approximately 20percent of individuals in this population require mechanical support at a gestational age of 30 weeks. Lower birthweight infants are even more likely to require ventilatory support.
At less than 30 weeks’ gestation, neonates are unable to maintain normal intrapulmonary pressures because of their inability to produce adequate amounts of surfactant. High levels of supplemental oxygen are often required until replacement surfactant is delivered. At 26 to 28 weeks’ gestation, the system that transports oxygen to the vital areas of the body is also impaired. Alveolar collapse (along with immature pulmonary capillaries) greatly reduces the ability of the pulmonary/ cardiovascular system to exchange gases.2
Bronchopulmonary dysplasia (BPD) is a major cause of infant mortality and morbidity in low-birthweight infants. Premature infants weighing 500 g to 1 kg have a 60percent chance of developing BPD. Premature infants in this weight category who require ventilatory support during the first 3 days of life have an 80percent chance of developing BPD.3
Early respiratory intervention is recommended. Surfactant should be administered within 15 minutes of birth, if not in the delivery room itself. Lung compliance will be affected by the surfactant immediately, and this changed compliance will help the practitioner determine which ventilator settings are appropriate. Ventilator selection, mode, timing, and strategy will, in turn, determine the level of pulmonary complication seen in the critically premature infant. Several ventilatory support modes can be employed; these include pressure-limited time-cycled ventilation, volume-controlled ventilation, high-frequency ventilation, bilevel positive airway pressure, and continuous positive airway pressure. Implementing a total-support strategy package at the earliest possible time will reduce the level of BPD seen later.4
Diseases such as subglottic stenosis, tracheal stenosis, and tracheobronchomalacia can substantially increase the work of breathing, calling for the use of higher ventilatory pressures and uniform flow patterns. Extubation of the infant in the recovery room should be cautiously monitored. Tracheostomy may be considered, in severe cases, for long-term airway management.5,6
A higher incidence of intracranial hemorrhage is seen in premature infants weighing less than 700 g.7 Its primary cause, in this particular group, is asphyxia. Several categories of intracranial bleeding have been identified in this population; all have the potential to affect and impair neurological status, which may, in turn, affect respiration. Blood pressure monitoring becomes a critical issue, therefore, when surgical procedures are unavoidable.
Basic considerations
Assessments of the infant’s preoperative condition and surgical needs are most important to the anesthetist. The infant’s history, gestational age, and weight are prerequisite information for surgical procedures. Data accumulated by attending physicians, nurses, and RCPs provide valuable insight into conditions that may determine the type, method, and strategic approach of anesthesia.8,9
Congenital defects may, in themselves, place the infant in a high-risk category. There may also be multiple defects that create intubation difficulties. Esophageal reflux and the aspiration of gastric contents may occur during a procedure. A nasogastric tube should be inserted in all neonates undergoing anesthesia. This is especially important if an intestinal obstruction is evident. The prevention of aspiration and basal atelectasis is of paramount concern.10,11
Anesthesia
The premature infant presents unique physiology, anatomy, and pathology and requires focused strategies for presurgical management and for the administration of anesthesia. Unique, major risk factors such as thermal instability, cardiac depression, airway-management dehydration, and nutritional demands validate the need for a high-risk patient profile.
Preparation for the administration of anesthesia is necessary, and it includes the maintenance of a neutral thermal environment in the operating room. Prewarmed heating pads and warming covers should be readily available in order to reduce the infant’s oxygen consumption and prevent cardiopulmonary suppression resulting from the metabolic response to cold. Increased work of breathing may be caused by improper thermal maintenance and may lead to glucose imbalance. Inspired gases, as well as blood fluids, should be warmed in order to guarantee thermal stability. Inadequate thermoregulation may lead to cardiovascular depression and hypotension.
There is a greater risk of cardiovascular collapse during anesthesia for the very small premature infant than for the full-term infant. Cardiac output in the very small premature infant cannot increase as much, or as rapidly, because of a high resting heart rate. Therefore, a higher risk of hypovolemia, hypotension, and shock exists. Anesthesia also blunts baroreflexes.12 In short, limited ventricular capacity, high heart rate, low blood volume, and undeveloped autoregulation place the very small premature infant in a high-risk category.
In this infant population, both airway management methods and lung physiology can create conditions that predispose the patient to obstruction. Intubation is required for most surgical procedures after anesthetics or nonpolarizing muscle relaxants are administered.
Risk factors associated with smaller airways (including 2.5-mm and 3-mm endotracheal tubes) include higher airway resistance, flow impedance, and waveform patterns (loops) as displayed on graphic monitors. Salem et al1 found that airway obstruction, accidental extubation, and esophageal intubation were responsible for half of cardiac arrests in a series of 73 such surgical occurrences. A precisely placed, secure endotracheal tube is important in order to ensure a stable cardiopulmonary environment during the surgical procedure. The risk of bronchospasm caused by the movement of an unstable endotracheal tube is high in the very small premature infant with preexisting pulmonary disease.
Younger gestational ages place premature infants at a disadvantage in maintaining normal body fluid levels. Fluid overloads and deficits are common, as renal function is less effective in prematurity. Close monitoring of this system is necessary in order to prevent dehydration or fluid overload.
Closely associated with fluid balance is nutrition, which can be equated with available energy. Premature infants have compromised energy levels, and this is a physiologic risk factor. Workloads become serious stressors, and high metabolic rates deplete the resources required for growth and development, with life-threatening consequences for a premature infant. The surgical team, therefore, must monitor electrolyte and fluid balances closely
Inhaled Anesthetics
Several inhaled anesthetics are currently in use, including isoflurane, enflurane, halothane, sevoflurane,desflurane, and nitric oxide. Of these, isoflurane is preferred because less is required, cardiovascular depression is reduced, and superior recovery characteristics are associated with it.13
Combinations of inhaled anesthetics, muscle relaxants, barbiturates, and narcotics are now used for their individual properties and combined effects. Nitric oxide, combined with more volatile agents such as halothane, enflurane, and isoflurane, also produces less cardiovascular depression.13
Regional Anesthesia
Studies14,15 have indicated that regional anesthesia is not to be considered as a sole anesthesia method for premature infants, but is beneficial as a supportive element when combined with general anesthesia. Smaller fractions of general anesthesia are required when regional anesthesia is used in conjunction with it. Titration, whenever and wherever possible, is recommended in order to ensure maximum effectiveness using minimal amounts of anesthesia. In this category, as for general anesthesia, a cardiovascular accident is the most common complication, regardless of the combination used.
Analgesics and Sedatives
In the past, there was controversy concerning whether the neonate experiences pain and, if so, at what threshold. There are reports16 indicating that premature infants do not experience the same amount of pain as an adult because their central nervous systems are immature. A 1988 survey conducted by Purcell-Jones et al17 indicated that 20 percent of physicians surveyed in the United Kingdom and Ireland doubted that infants less than a week old perceived pain. As a result, some surgical procedures were performed on unanesthetized or underanesthetized patients. Fortunately, the opinions responsible for that policy have changed. Recent scientific reviews and surveys17 indicate that the majority of physicians agree that neonates do perceive pain, and that the central nervous systems of premature infants are much more mature than previously thought. Data from the studies of Anand and Hickey18 indicate that surgical pain has definite physiological and behavioral effects on the neonate and that the use of anesthesia is necessary. In fact, physiological and behavioral instability can result from inadequate anesthesia, affecting the cardiac, circulatory, and metabolic systems.
Muscle relaxants alone are not considered pain-relieving agents. They are beneficial when used in conjunction with anesthesia, but care should be taken to recognize restrictions and interactions that can affect their use in this manner.
ANESTHESIA AND COMMON DISORDERS
Diaphragmatic Hernia
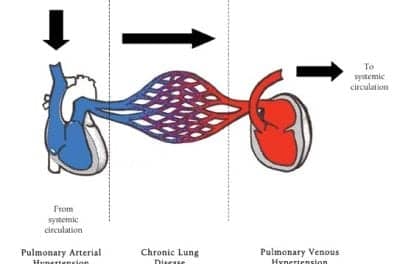
This is a drastic thoracic surgical emergency requiring immediate surgical response and management. Ventilatory and respiratory management are required in acute cases before the reduction of the hernia and the repair of the hemidiaphragm may begin. This anatomic congenital anomaly may compound the infant’s pulmonary stability by causing pulmonary hypertension and pulmonary parenchymal insufficiency, both of which create significant respiratory distress.19
The recommended anesthesia would be low-dose halothane or isoflurane with oxygen and intravenous fentanyl or morphine. Muscle relaxants may also be considered.
Patent Ductus Arteriosus
Patent ductus arteriosus occurs more often in premature infants than in the full-term population. Of premature infants with severe RDS who require mechanical ventilation, 70percent to 80percent are likely to have this problem. Pharmacological intervention using indomethacin is common and is effective in many cases. There are, however, those infants who require surgical assistance in order to correct the problem. Patent ductus arteriosus has been known to promote pulmonary hypertension or congestive heart failure. An echocardiogram can identify the disorder at an early stage, usually at an age of 3 to 5 days.
The recommended anesthesia would be isoflurane or desflurane in nitric oxide and oxygen. Muscle relaxants, along with narcotics, are also options for small infants with congestive heart failure.
Tracheoesophageal Fistula
The common characteristic of this problem is a connection between the esophagus and trachea. Gastric-contents aspiration, causing pneumonitis and bronchospasm, often results from this condition.20 Careful placement of the endotracheal tube is required. Prolonged postoperative endotracheal intubation with mechanical ventilation is often needed for premature infants with active lung disease.
The recommended anesthesia would be halothane, isoflurane, or desflurane in air and oxygen. The support of muscle relaxants may be considered.
Retinopathy of Prematurity
High concentrations of oxygen administered to a premature infant can cause the retinal vessels to constrict and become necrotic. Circulation will become impaired and obliteration of the retinal vessels can occur, causing impaired vision or blindness.21
Extreme caution must be taken in administering oxygen to the low-birthweight infant. Intensive care strategies should be formulated and implemented to reduce the oxygen requirements of the infant as soon as possible (in order to minimize damage to the retina). This is a critical factor for the anesthesiologist as well. The use of oxygen in the operating room requires close monitoring and titration.
Postoperative Care
There are obvious clinical concerns and risks associated with surgery in infants. Primary respiratory dysfunction can lead to postoperative complications that will require medical monitoring and intervention. One element of this situation requires a special focus: the patient’s parents need to be well informed concerning their infant’s status. The presurgical briefing should be followed, in due course, by a postsurgical progress and outcome report.22 Simple, nontechnical discussions explaining the nature of (and need for) the support and monitoring equipment in use will also help relieve anxieties and fears. Feelings of helplessness and isolation often overwhelm parents. Focusing parental attention on the infant, rather than on intimidating hardware, will help to create a more familiar environment.
An early understanding of the infant’s postoperative needs, both in the intensive care unit and at home, will assist parents during this adjustment period. Clinical and emotional support may be required and should be coordinated in association with the health care team.
Conclusion
Critically premature infants are unstable and challenging. Compromised physiology caused by unique disease processes and underdeveloped systems requires focused care and strategic thinking. The anesthesiologist and RCP play very important roles in the care of the premature infant. Patient outcomes are, in fact, dependent upon the performance and skill levels of these individuals. The degree of surgical risk present can be influenced by the presurgical care administered to the infant; the level of recovery can be affected by the surgical procedure. There exists an interdependent relationship between the two.
Premature infants cannot be classified. They may exhibit the same disease processes, levels of immaturity, and conditions of birth, but they are unique in their response to the care given to them. The health care team should never assume anything concerning this patient population. Its members are the ultimate challenge to those of us who choose to care for them.
Michael E. Donnellan, MBA, RRT, is a perinatal specialist at Sutter Alta Bates Medical Center in Berkeley, Calif.
References
1. Salem MR, Bennett EJ, Schwass JF, et al. Cardiac arrest related to anesthesia: contributing factors in infants and children. JAMA. 1975;1:233-238.
2. Diaz JH. Intraoperative management. In: Goldsmith JP, Karotkin HK, eds. Assisted Ventilation of the Neonate. 3rd ed. Philadelphia: W.B. Saunders; 1996:409-423.
3. Gomella TR. Neonatology Management, Procedures, On Call Problems, Diseases, Drugs. 2nd ed. New Jersey: Lange Clinical Manual; 1992:441-442, 446-447.
4. Korones SB. Complications: bronchopulmonary dysplasia, air leak syndromes, and retinopathy of prematurity. In: Goldsmith JP, Karotkin HK, eds. Assisted Ventilation of the Neonate. 3rd ed. Philadelphia: W.B. Saunders; 1996:327-330.
5. Gomella TR. Neonatology, Management, Procedures, On Call Problems, Diseases, Drugs. 2nd ed. New Jersey: Lange Clinical Manual; 1992:114.
6. Gomella TR. Neonatology, Management, Procedures, On Call Problems, Diseases, Drugs. 2nd ed. New Jersey: Lange Clinical Manual; 1992:413-417.
7. Powers L, Burrington J, Gardner S, Merenstein GB. Pediatric surgery. In: Merenstein GB, Garden SL, eds. Handbook of Neonatal Intensive Care. 2nd ed. St Louis: CV Mosby; 1989:554-557.
8. Hatch D, Summer E, Hellmann J. The Surgical Neonate: Anaesthesia and Intensive Care. 3rd ed. Boston: Edward Arnold Group; 1995:120-121, 138-142.
9. Hatch D, Summer E, Hellmann J. The Surgical Neonate: Anaesthesia and Intensive Care. 3rd ed. Boston: Edward Arnold Group; 1995:150-151.
10. Fluck JR. Congenital cardiovascular diseases. In: Aloan CA, Hill TV, eds. Respiratory Care of the Newborn and Child. 2nd ed. Philadelphia: Lippincott; 1997:227-229.
11. Aloan CA, Hill TV. Respiratory Care of the Newborn and Child. 2nd ed. Philadelphia: Lippincott; 1997:255-256.
12. Spaeth JP, O’Hara IB, Kurth CD. Anesthesia for the micropremie. Semin Perinatol. 1998;22:390-401.
13. Welborn LG, Greenspun JC. Anesthesia and apnea. Pediatr Clin North Am. 1994;41:181-193.
14. Push F, Wilding E, Grabner SL. Principles in Peri-Operative Paediatric Medicine. Vienna: University of Vienna; 1992:45-48.
15. Daberkow E, Washington RL. Cardiovascular diseases and surgical interventions. In: Merenstein GB, Garden SL, eds. Handbook of Neonatal Intensive Care. 2nd ed. St Louis: CV Mosby; 1989:433-437.
16. McLaughlin CR, Hull JG, Edwards WH, Cramer CP, Dewey, WL. Neonatal pain: a comprehensive survey of attitudes and practices. Journal of Pain and Symptom Management. 1993;8:8-14.
17. Purcell-Jones G, Dorman F, Summer E. Paediatric anaesthetists perceptions of neonatal and infant pain. Pain. 1988;33:181-187.
18. Anand KJS, Hickey PR. Pain and its effects in the human neonate and fetus. N Engl J Med. 1987;317:1321-1329.
19. Leveque C, Jamil H, Berg AE, et al. Successful repair of a severe left congenital diaphragmatic hernia during continuous inhalation of nitric oxide. Anesthesiology. 1994;80:1171-1175.
20. Aloan CA, Hill TV. Respiratory Care of the Newborn and Child. 2nd ed. Philaelphia: Lippincott; 1997:152-158.
21. Hagedorn MI, Gardner SL, Abman SH. Respiratory diseases. In: Merenstein GB, Gardner SL, eds. Handbook of Neonatal Intensive Care. 2nd ed. St Louis: CV Mosby; 1989:396-399.
22. Troug R, Arnold KJS. Management of pain in the post-operative neonate. Clin Perinatol. 1989;16:61-78.