Capnography has long been a tool used by RTs to monitor ventilation in the ICU. With the release of the new Advanced Cardiovascular Life Support (ACLS) and Pediatric Advanced Life Support (PALS) guidelines from the American Heart Association (AHA), capnography has now become the standard of care for use by “Code Teams.”
On October 18, 2010, the AHA guidelines were released along with new guidelines from the International Liaison Committee on Resuscitation (ILCOR) and European Resuscitation Council (ERC). This update to the 2005 guidelines was prompted by input from 356 resuscitation experts from 29 countries who reviewed, analyzed, evaluated, debated, and discussed research and hypotheses through in-person meetings, teleconferences, and online sessions (webinars) during the 36-month period leading up to the 2010 Consensus Conference.
With the release of the new AHA guidelines, hospitals and other facilities following ACLS/PALS guidelines will need to ensure that “crash carts” are equipped with capnography monitors to comply with AHA standards. Advanced Cardiovascular Life Support trainers are currently rewriting curricula to ensure that they follow the new ACLS recommendations for using quantitative waveform capnography, which will also need to be reflected in hospital policies.
The “2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care” call for the use of waveform capnography (etCO2 monitoring) during CPR to confirm and monitor endotracheal tube placement, assess the quality of CPR, and detect return of spontaneous circulation (ROSC).1
Capnography has long been the American Society of Anesthesiologists (ASA) standard of care in the operating room to monitor ventilation for patients receiving general anesthesia. In October, the ASA also enacted a recommendation to monitor end-tidal CO2 during moderate or deep sedation procedures.2 The 2010 AHA guidelines are just the latest validation of the importance of capnography in saving lives outside of the operating room.
Using Capnography During Resuscitation
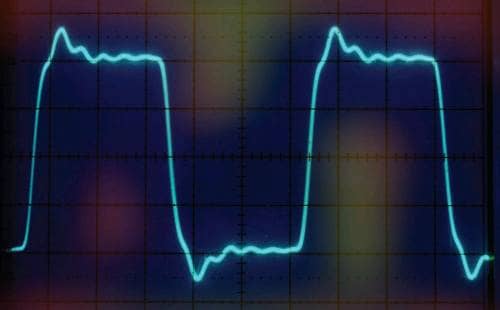
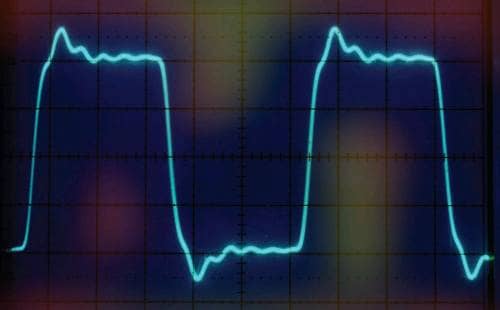
Traditionally, etCO2 has been used by RTs to monitor ventilation for intubated patients in the ICU. Capnography provides an accurate “physiologic” respiratory rate, while end-tidal CO2 values provide an indication of the adequacy of ventilation. Capnography waveforms, the graphic representation of exhaled CO2, offer the clinician an immediate indication of apnea or other airway compromise. The shape of the capnograph has even been determined to have diagnostic values.3 However, during resuscitation, the role of capnography serves additional purposes.
- Confirming ET Tube Placement. Measuring for the presence of exhaled CO2 in the endotracheal (ET) tube serves to confirm the placement of the tube in the trachea. The AHA guidelines state, “Continuous waveform capnography is recommended in addition to clinical assessment as the most reliable method of confirming and monitoring correct placement of an endotracheal tube.”
In addition to confirming initial ET tube placement, capnography also serves to monitor that the ET tube placement is being maintained in the trachea. It is not uncommon for the tube to become dislodged during the activity surrounding resuscitation or during transport after. AHA guidelines recommend, “Providers should observe a persistent capnographic waveform with ventilation to confirm and monitor endotracheal tube placement in the field, in the transport vehicle, on arrival at the hospital, and after any patient transfer to reduce the risk of unrecognized tube misplacement or displacement.”
- CPR Quality and ROSC Detection. The AHA recommends quantitative waveform capnography in intubated patients to monitor CPR quality, optimize chest compressions, and detect ROSC.
Blood must circulate through the lungs for CO2 to be exhaled and measured. During resuscitation, etCO2 assesses the adequacy of chest compressions by noninvasively monitoring pulmonary blood flow. Low etCO2 suggests inadequate pulmonary blood flow or poor chest compressions, whereas higher etCO2 can reflect improved compressions. If etCO2 is <10 mm Hg, the AHA suggests trying to improve CPR quality by optimizing chest compression. When there is a dramatic sustained increase in etCO2 (typically >40 mm Hg), it signals ROSC.
- Capnography in PALS. The AHA also recommends continuous capnography during pediatric CPR to confirm ET tube placement, to assess the quality of CPR, and as an indication of ROSC. They state, “PetCO2 values consistently <10 to 15 mm Hg suggest that efforts should be focused on improving chest compressions and making sure that ventilation is not excessive. An abrupt and sustained rise in PetCO2 may be observed just before clinical identification of ROSC, so use of PetCO2 monitoring may reduce the need to interrupt chest compressions for a pulse check.”
Capnography Use Before the Code
Respiratory depression is the number one reason for “codes” in hospitals4 and the most common antecedent of in-hospital cardiac arrest.5 Although the new AHA guidelines specifically address resuscitation, capnography can also be utilized by rapid response teams during patient assessment as an early indication of respiratory distress. Rapid response teams are called when a patient experiences an acute change in status, such as rapid or slow heart rate, extremely high or low respiratory rate, low blood pressure, low oxygen saturation, or deterioration in alertness.
The goal of the teams is to prevent further decline, keeping the patient from “coding,” or declining into cardiac arrest. The first order of the team is patient assessment, including assessment of the patient’s breathing. Without capnography, clinicians assess breathing with pulse oximetry (oxygenation status) and measurement of respiratory rate (the number of breaths). But neither pulse oximetry nor respiratory rate, together or alone, monitors adequacy of ventilation: how well the patient is breathing. Capnography, along with oximetry, provides a complete measure of the patient’s ventilation and oxygenation.
Summary
Capnography’s role outside of the OR continues to grow and evolve. As a result of the 2010 AHA guidelines, continuous quantitative waveform capnography is now recommended for intubated patients throughout the peri-arrest period. When quantitative waveform capnography is used for adults, applications now include recommendations for confirming endotracheal tube placement and for monitoring CPR quality and detecting ROSC based on etCO2 values. Hospital RT departments should take the lead in patient safety by ensuring that their facilities are in compliance with these important new recommendations.
The full guidelines are available at [removed]static.heart.org/eccguidelines/2010-guidelines-for-cpr.html[/removed].
Greg Spratt, BS, RRT, CPFT, is director of clinical marketing, Oridion Capnography, Needham, Mass. For further information, contact [email protected].
References
- American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC). Highlights of the 2010 American Heart Association Guidelines for CPR and ECC. Available at: [removed]www.heart.org/idc/groups/heart-public/@wcm/@ecc/documents/downloadable/ucm_317350.pdf[/removed]. Accessed March 21, 2011.
- ASA Standards for Basic Anesthetic Monitoring. Available at: www.asahq.org/For-Healthcare-Professionals/Standards-Guidelines-and-Statements.aspx. Accessed March 21, 2011.
- Krauss B, Heightman AJ. 15-Second triage tool. JEMS. 2006;31:60-8.
- Fecho K, Joyner L, Pfeiffer D. Opioids and code blue emergencies. Anesthesiology. 2008;109:A34.
- Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. CHEST. 1990;98:1388-92.